A larger genetic inventory may help explain how certain dangerous bacteria can persist in a hospital environment and continue to infect patients, according to a new study in the journal Proceedings of the National Academy of Sciences.
In their paper published on Thursday, researchers including Dr. Jeffrey McLean of the UW School of Dentistry describe their discovery that three closely related species of bacteria of the family Enterobacteriaceae outlived all other oral bacteria in a long-term starvation or “doomsday” experiment.
“A number of species from that family are known to cause infections in hospitals,” said Dr. Xuesong He, an associate member of staff at the Forsyth Institute of Cambridge, Mass., and co-author of the study. Other team members were from the University of California, Los Angeles, and the J. Craig Venter Institute of La Jolla, Calif., and Rockville, Md.
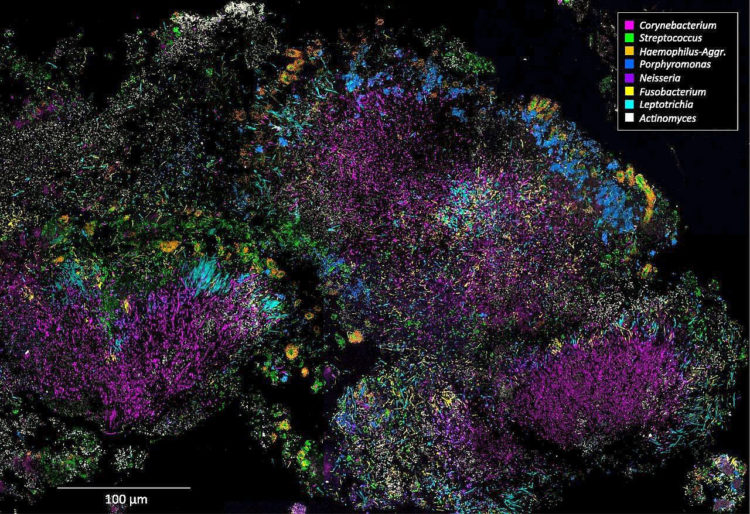
More than 200 different bacterial species live inside your mouth. Some are highly abundant, while others are scarce. A few of these oral bacteria are known pathogens, which can cause disease. However, most are harmless or even beneficial.
Scientists know the genetic makeup of about 70% of oral bacteria. What they don’t know is which species would be most successful in surviving long-term starvation — so they decided to find out.
To create a battle of bacteria, researchers placed a community of oral bacteria, derived from human saliva, into a mixture of sterilized saliva and saline solution. The bacteria, which are accustomed to living in the nutrient-rich mouth, were starved in their new environment. Every few days, scientists checked the samples to see which bacteria were still alive.
Nearly every bacterial species died within the first couple of days. But three species — Klebsiella pneumoniae, Klebsiella oxytoca, and Providencia alcalifaciens — survived the longest, with K. pneumoniae and P. alcalifaciens surviving for more than 100 days.
Researchers were surprised to find that Klebsiella were among the champions of this bacterial combat. In the mouth, Klebsiella are considered an underdog, accounting for only about 0.1% of all microbes there. But in an extreme environment deprived of all nutrients, Klebsiella gained superiority, while the bacterial populations normally found in high abundance died off rapidly.
“When we look at the genome content, it turns out that these Enterobacteriaceae species have larger genomes than other oral bacteria, giving them the capacity to tap into more diverse energy sources,” said Dr. He.
To begin to understand how Klebsiella pulled off such a feat, scientists analyzed the genome of the bacteria on the first day of “battle” and then again on day 100. They found that the Klebsiella had undergone genetic mutations that may have allowed them to survive and continue to function, even without a food source.
“Oral fluids like saliva are a rich source of bacteria and viruses,” said Dr. McLean, another co-author of the study and an associate professor of periodontics at the School of Dentistry. “We want to understand how pathogens that are typically rare can become dominant and then also persist for long periods outside the body to be later transmitted.”
Scientists describe Klebsiella species as opportunistic pathogens. In healthy people, they live in the mouth peacefully, crowded by other microbes and are unable to grow or cause trouble. But outside the mouth, where few other oral bacteria survive, Klebsiella is king.
The species persists on hospital surfaces, like sinks or tables. Patient with compromised immune systems who contact the Klebsiella can develop infections that can lead to such dangerous conditions as pneumonia, meningitis, or septicemia. Pneumonia caused by Klebsiella has a very high death rate of around 50%. One reason why Klebsiella infections are so dangerous is that these bacteria are particularly adept at developing resistance to antibiotics, as well as transferring this drug resistance to their neighbors.
“The finding that these Klebsiella species survive longer than their more benign neighbors in mixtures of saliva is likely to have a great deal of clinical significance, as multiple virulent outbreaks of antibiotic-resistant Klebsiella have been traced back to hospital sinks and drains,” said Dr. Jonathon Baker. Dr. Baker is a Ruth L. Kirschstein NRSA Fellow at the J. Craig Venter Institute and lead author of the study.
The techniques employed in this research are key to illuminating the ecological dynamics of bacterial communities.
“From a big-picture point of view, this is a huge step forward toward understanding microbial social structure and ecology,” said Dr. Wenyuan Shi, CEO and chief scientific officer at the Forsyth Institute. “This study begins to address a fundamental question in biology: How, evolutionarily, was a microbial community built, and what takes place as the community dies?”