Return to Case of the Month Archives
Severe localized periodontitis; right posterior mandible
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Contributed by
Dr. David Cotant
Lakewood Oral Surgery, Lakewood, WA
Case Summary and Diagnostic Information

This is a 27-year-old white male who presented with less than a year history of a lesion in the posterior mandible with symptoms of pain, gingival swelling, and ulceration around teeth #s 29-31.
Diagnostic Information Available
This is a 27-year-old white male who presented with less than a year history of a lesion in the posterior mandible with symptoms of pain, gingival swelling, and ulceration around teeth #s 29-31. The patient was aware of the symptoms for only a few months. The gingiva around these teeth was grey-purple and showed extensive recession (Figure 1). The panoramic radiographic findings (Figure 2) notably show extensive bone loss with the appearance of teeth “floating in space.” He was treated with Amoxicillin and Flagy to no avail. Recent bone scan showed a small lesion in the right rib and possibly some very small lesions in the skull.

Figure 1 Photograph taken at first clinical presentation. Note the severe periodontitis with gingival recession involving teeth #s 29-31

Figure 2 Panoramic radiograph taken at first clinical presentation. Note the sharply demarcated lytic lesion of teeth #s 29-31 giving the impression of teeth “floating” in space.e
The past medical history is significant for pituitary gland swelling and diabetes insipidus. Family history is negative.
Clinical examination revealed severe localized soft tissue and bone destruction in form of severe localized periodontitis affecting teeth #s 29-30 which had three plus mobility. The gingiva was purplish and showed significant recession (Figure 1). The panoramic radiograph (Figure 2) revealed teeth “floating” in space with extensive bone resorption. All three teeth were extracted and the soft tissue submitted for microscopic evaluation.

Figure 1 Photograph taken at first clinical presentation. Note the severe periodontitis with gingival recession involving teeth #s 29-31

Figure 2 Panoramic radiograph taken at first clinical presentation. Note the sharply demarcated lytic lesion of teeth #s 29-31 giving the impression of teeth “floating” in space.
Treatment
Under local anesthesia, teeth #s 29-31 were extracted and the area thoroughly curetted. Post operative healing was yielding good results. However on the seventh week, the patient returned with small red-purplish areas (Figure 3) in the healing sockets. The lesions were re-biopsied to reveal residual pathology. The area was curetted and the patient is healing well since.
Incisional and excisional biopsy
Histological examination revealed sheets and clusters of large cells with abundant cytoplasm and folded, grooved or bean shaped nuclei intermixed with many eosinophils and a few multinucleated giant cells (Figures 4 & 5). The immunohistochemistry stain showed strong membrane expression with CD1a antibody (Figure 6) and uniform nuclear and cytoplasmic positivity with S-100 antibody (Figure 7). A few mitotic figures were identified.
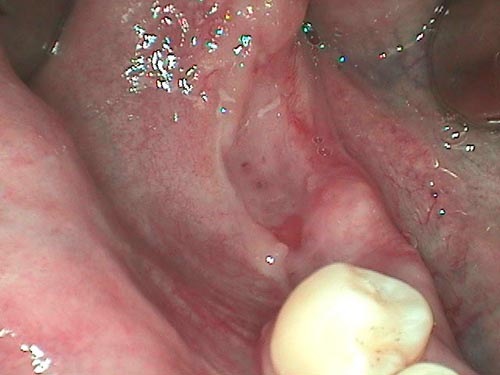
Figure 3 Photograph taken seven weeks post extraction and curettage. Note the small red areas overlying the healing socket.
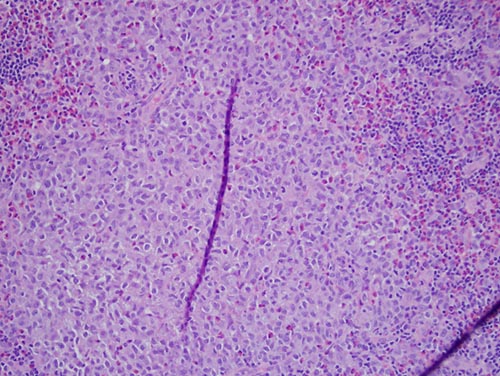
Figure 4 Low power (x100) H & E histology shows clusters of large round cells with abundant cytoplasm and bean-shaped and folded nuclei intermixed with many eosinophils.
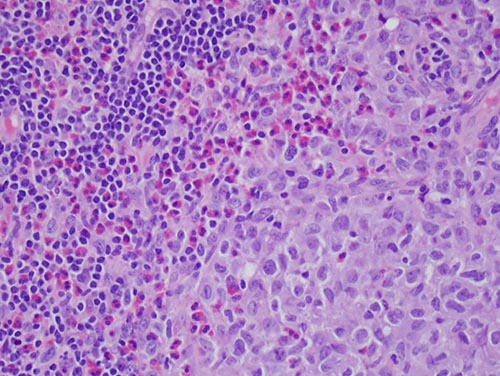
Figure 5 High power (x200) H & E histology shows clusters of large cells with abundant cytoplasm and folded nuclei intermixed with many eosinophils.
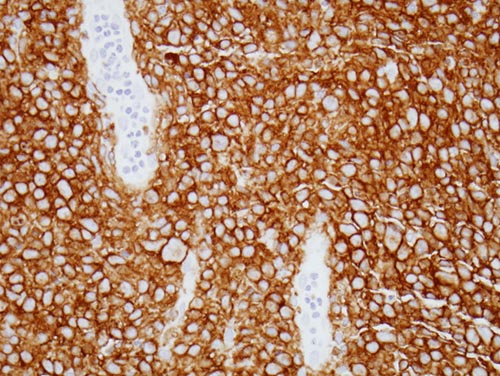
Figure 6 High power (x200) immunohistochemistry stain with CD1a antibody. Note the uniform and strong cell membrane positive stain.
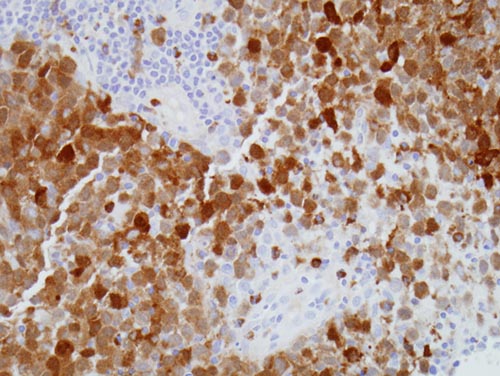
Figure 7 Low power (x100) immunohistochemistry stain with S-100 protein antibody. Note the uniform and strong nuclear and cytoplasmic positive stain.
After you have finished reviewing the available diagnostic information