Return to Case of the Month Archives
October 2010: Recurring Lobular Exophytic Lesion Right Lateral Tongue
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Contributed by
Drs. A. Estess & R. Beirne
University of Washington, Seattle, WA
Case Summary and Diagnostic Information

This is a 49-year-old white female who was referred to the University of Washington, Department of Oral Surgery for a fast-growing, recurring, exophytic mass on the right lateral border of tongue present since August 2008.
This is a 49-year-old white female who was referred to the University of Washington, Department of Oral Surgery for a fast-growing, recurring, exophytic mass on the right lateral border of tongue (Figure 1) present since August 2008. This lesion recurred in January 2010 and was excised again in April 2010. The lesion persisted after the second surgery and was reported to be painful. The lesion is frequently traumatized by the adjacent dentition which is in a poor state of repair, including malocclusion and sharp/irregular teeth with broken restorations. A mandibular mouth guard was fabricated; however, due to the large size of the lesion, the mouth guard did little to prevent occlusal trauma. This lesion was excised in June 2010 for a third time under general anesthesia.

Figure 1 This photograph demonstrates an exophytic, lobular and pink to red and focally ulcerated mass on the right lateral and ventral surfaces of tongue.
The patient’s past medical history is significant for Hepatitis C, rheumatoid arthritis, fibromyalgia, migraines, GERD, depression and chronic pain. Her medications include Dilaudid, Morphine, Promethazine, Maxalt, Omeprazole, Sertraline, Zithromax, Wellbutrin, flax seed oil and black cohosh caps. She is a former smoker.
In August 2008, the patient presented with an exophytic lobular mass on the right lateral border of tongue, which was excised. It recurred in January 2010 (Figure 1) and was excised again in April 2010. The lesion persisted after the second surgery and was reported to be painful. A mandibular mouth guard was fabricated; however, due to the large size of the lesion, the mouth guard did little to prevent occlusal trauma. This lesion was excised in June 2010 for a third time under general anesthesia.

Figure 1 This photograph demonstrates an exophytic, lobular and pink to red and focally ulcerated mass on the right lateral and ventral surfaces of tongue.
Treatment
The first two excisional surgical procedures were performed under local anesthesia. The last procedure was performed under general anesthesia. Bupivacaine, 1:200,000 parts epinephrine was administered to the site via infiltration; a total of 10 mls. Needlepoint electrocautery and tissue forceps were used to completely excise the body of the lesion. Hemostasis was easily achieved with electrocautery. The site was thoroughly irrigated and the wound reapproximated with 3-0 Vicryl sutures, which were buried and placed in an interrupted fashion. The wound was hemostatic at the end of the procedure.
Incisional Biopsy
This biopsy was read by Dr. Thomas Morton of the Oral Pathology Biopsy Service, University of Washington. Histologic examination reveals a multisected piece of soft tissue composed of ulcerated surface epithelium with underlying fibrous and granulation tissue supported by skeletal muscle bundles (Figure 2). The ulcerated surface is covered by fibrin, neutrophils and cellular debris (Figure 3). The epithelium next to the ulcer shows evidence of reactive atypia but the remaining surface epithelium is benign with no evidence of neoplastic changes. The granulation tissue below the ulcer is infiltrated by many lymphocytes, plasma cells, neutrophils and eosinophils (Figure 4). The granulation tissue and the inflammatory cells extend deeply into the underlying skeletal muscle bundles (Figure 5).
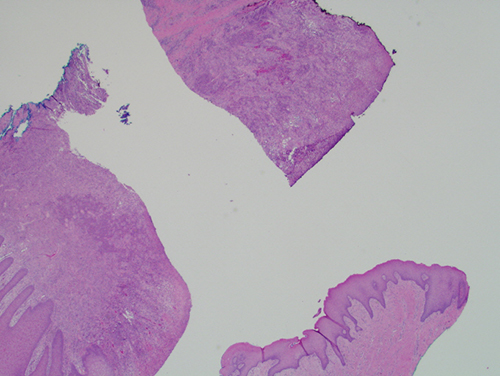
Figure 2 Low power (x40) the H & E histology reveals a multisected piece of soft tissue exhibiting surface ulceration with underlying granulation tissue intensely infiltrated by inflammatory cells. The surface is covered by fibrin and neutrophils. Where present, the epithelium is hyperplastic but benign and well-differentiated.
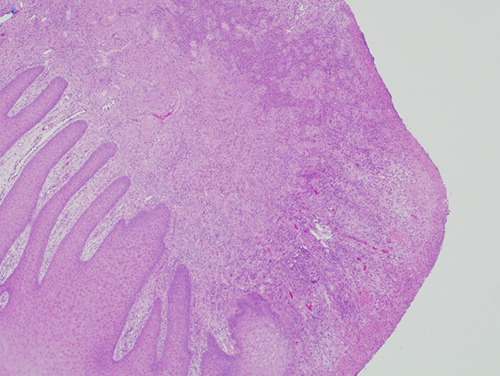
Figure 3 Low power (x100) the H & E histology with a closer look at the ulcerated surface epithelium. The intact epithelium is hyperplastic and well differentiated.
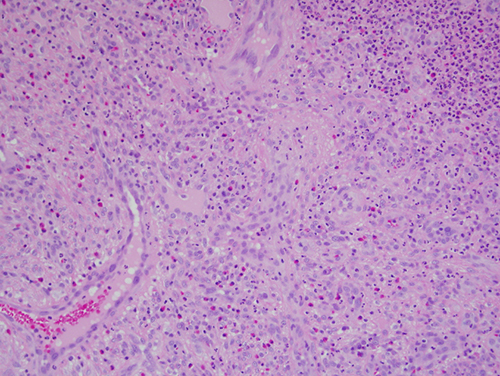
Figure 4 High power (x200) the H & E histology with a closer look at the granulation tissue constituting the ulcer bed infiltrated by many neutrophils and eosinophils.
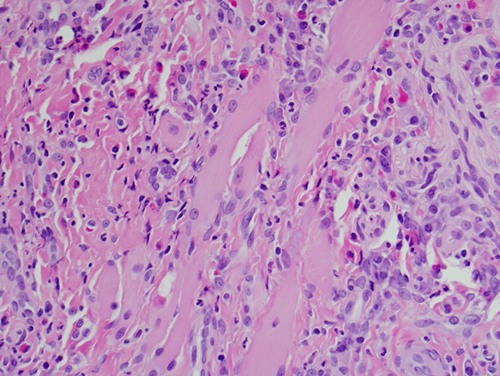
Figure 5 High power (x200) the H & E histology with a closer look at the intramuscular inflammatory infiltrate.
After you have finished reviewing the available diagnostic information