All cases are discussed by: Dr. Dolphine Oda, UW-Oral Pathology Biopsy Service
Expansile, mixed RL/RO lesion associated with impacted tooth #18
Contributed by: Drs. Ross Beirne & William Alvarez, Oral & Maxillofacial Surgery, UWSOD, Seattle, WA
Case Summary and Diagnostic Information
This is a 26-year-old female who had a panoramic radiograph taken in 2011 which showed an impacted tooth #18 associated with a mixed radiolucent-radiopaque lesion.
This is a 26-year-old female who had a panoramic radiograph taken in 2011 which showed an impacted tooth #18 associated with a mixed radiolucent-radiopaque lesion. The patient states that she “did not follow up on it” until January 2017, at which point she felt occasional pain. Extra-oral examination showed a symmetrical jaw while intra-oral examination showed lingual expansion at the left body of the mandible (Figure 3). All third molars were impacted, as was tooth #18. There was supra-eruption of tooth #15.
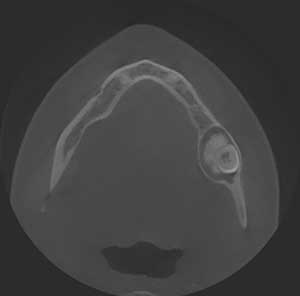
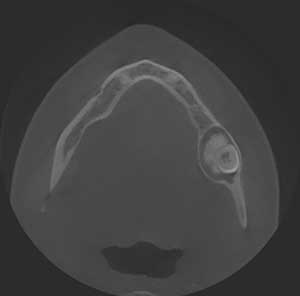
Figure 3 This is a CT axial scan view taken in 2017. It shows a clear lingual expansion and very little buccal expansion of this large well-circumscribed/corticated radiolucency associated with a larger radiopaque mass.
The patient’s past medical history is not contributory.
Two panoramic radiographs six years apart show an impacted tooth #18 associated with a mixed RL/RO lesion (Figures 1 & 2). The lesion increased in size over that time and became slightly symptomatic in early 2017. The radiographic changes demonstrate a well-demarcated and corticated mixed RL/RO lesion slowly enlarging over a six-year period. Extra-orally, the swelling was not noticeable. Expansion of the lingual bone in the left body of the mandible around teeth #s 17 and 18 was clinically visible (Figure 3). Tooth #15 was supra erupted.

Figure 1 This is a panoramic view taken in 2011. It shows impacted tooth #18 associated with a well-circumscribed/corticated radiolucency with a small radiopaque mass. Tooth #15 is slightly supra-erupted.

Figure 2 This is a panoramic view taken in 2017. It shows impacted tooth #18 pushed further inferiorly. This tooth is associated with a large lesion compared to 2011. This lesion is again a well-circumscribed/corticated radiolucency associated with a much larger radiopaque mass. Tooth #15 is clearly supra-erupted.
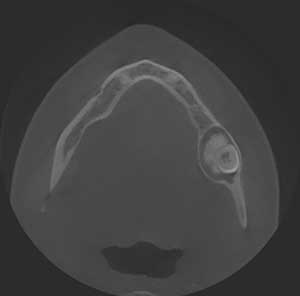
Figure 3 This is a CT axial scan view taken in 2017. It shows a clear lingual expansion and very little buccal expansion of this large well-circumscribed/corticated radiolucency associated with a larger radiopaque mass.
Under general anesthesia, teeth #s 1, 15, 16, 18 and 32 were extracted and the lesion associated with impacted tooth #18 was completely excised. The specimen removed from area of tooth #18 was submitted for histologic evaluation.
Histologic examination reveals multiple pieces of decalcified hard and soft tissue composed of a benign neoplasm of odontogenic epithelial origin (Figures 4-6). This neoplasm is made up of sheets of epithelial cells with abundant cytoplasm and round to oval nuclei joined together by intercellular bridges (Figures 5-6). Interspersed between the neoplastic epithelial cells were globules of eosinophilic material (Figure 4-6), some undergoing calcifications in form of rings (Figure 6). The eosinophilic material was positive with Congo red, apple-green with polarized light.
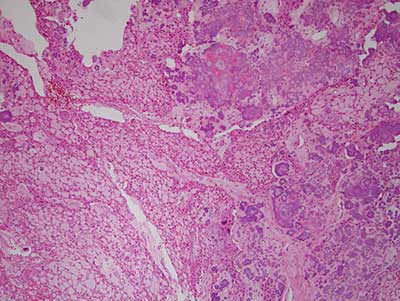
Figure 4 Low power (x100) H & E stained histology shows a large lesion with sheets of epithelial cells, eosinophilic smooth coagulum and calcified material.
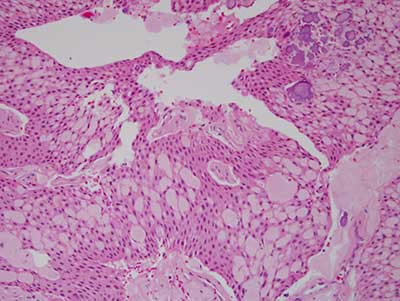
Figure 5 Higher power (x200) H & E stained histology shows a closer look at the epithelial cells attached with intercellular bridges and interspersed with eosinophilic and calcified material.
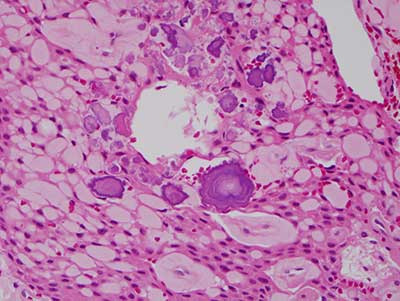
Figure 6 Higher power (x200) H & E stained histology shows a closer look at the eosinophilic material and the calcified material, some arranged in form of rings.
After you have finished reviewing the available diagnostic information