Single grayish blue swelling associated with an implant
Can you make the correct diagnosis?
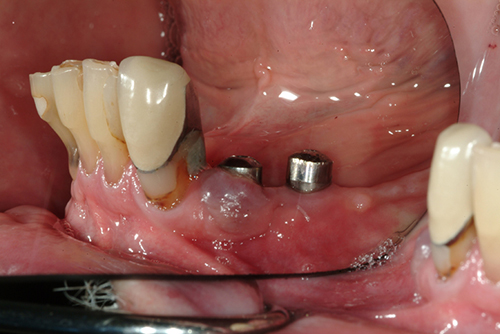
TThis 66-year-old white male presented to the Department of Periodontology, School of Dentistry complaining of a swelling of one year’s duration associated with an implant in the area of tooth #28.
Sorry! you are incorrect
Pyogenic granuloma constitutes 85% of all reactive gingival swellings, representing a profuse mass of vascular granulation tissue (1). It can be induced by local irritants such as excessive plaque, sharp fillings and dental calculus; it sometimes forms in an extraction socket in response to an irritant left in the socket. It can occur anywhere in the oral cavity and skin, especially the tongue, lips, fingers and nail beds (1). In the mouth, it occurs most commonly in the gingiva, especially the maxillary buccal and interproximal gingiva (1-2). Occasionally, it may surround the tooth. It is usually highly vascular, fast-growing, exophytic, lobular, sessile, and ulcerated or covered by pseudomembrane. The color changes from red to pink when it starts to heal. It occurs at any age and sex with a slight predilection for young females; it affects 1% of pregnant females. Pyogenic granuloma is usually painless except during eating, when bleeding and pain is described (1). Histologically, it presents as a mass of loose and vascular granulation tissue, usually with ulcerated or eroded surface epithelium and many inflammatory cells. A range of treatment modalities are available, including excision with removal of the local irritant, laser surgery, or intralesional injection with absolute alcohol, steroids or botulinum toxin (2-3). Scaling and polishing prior to surgical removal helps shrink the lesion. The prognosis is good, although recurrence is possible, especially during pregnancy.
Congratulations! You are correct
Peripheral giant cell granuloma constitutes less than 5% of all reactive gingival swellings, and consists of a hyperplastic mass of vascular granulation tissue with many osteoclast-like multinucleated giant cells. It presents as a lobular, purplish-blue exophytic nodule exclusively on the gingiva, both edentulous and dentate, and usually anterior to the molars (4-5). It originates from either the periodontal ligament or the periosteum. It occurs across a wide age range, especially in children, young adults, and females (2:1 female to male ratio) (4-6). It presents as either sessile or pedunculated and smooth surfaced or lobular; though usually painless, it can occasionally be ulcerated, painful and accompanied by bleeding (4-6). Like pyogenic granuloma, it is usually present either on the buccal or lingual gingiva or between teeth, but it can occasionally surround the teeth (4-6) and act aggressively by displacing teeth much like a sarcoma (4). It can also resorb the underlying bone in a smooth and concave “saucer-like” manner. Complete excision including curettage of underlying bone is the preferred treatment. It has a good prognosis with recurrence rate of approximately 10% (6).
Treatment
Under local anesthesia (2 x Lidocaine 1.100,000), the lesion was completely excised using a 15c blade, leaving 1mm of normal-looking keratinized tissue on the buccal of the implant. The specimen was placed in formalin and submitted for microscopic examination. The area was sutured with 5-0 plain gut suture. A one-week follow-up visit revealed that the area was healing well and that the gingiva around the implant had healed, but a small surface ulceration was present. Also present was a small area of purple-colored gingiva (Figure 2).
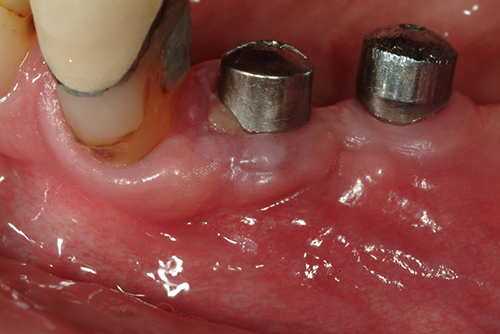
Figure 2. One week after the excisional biopsy, the gingiva shows good healing but a small surface ulceration is still present. Also note the small grayish discoloration on the buccal gingiva.
References
- Fantasia JE, Damm DD. Red nodular lesion of tongue. Pyogenic granuloma. Gen Dent. 2003 Mar-Apr;51(2):190, 194.
- Ichimiya M, Yoshikawa Y, Hamamoto Y, Muto M. Successful treatment of pyogenic granuloma with injection of absolute ethanol. J Dermatol. 2004 Apr;31(4):342-4.
- Pham J, Yin S, Morgan M, Stucker F, Nathan CA. Botulinum toxin: helpful adjunct to early resolution of laryngeal granulomas. J Laryngol Otol. 2004 Oct;118(10):781-5.
- Flaitz CM, Peripheral giant cell granuloma: a potentially aggressive lesion in children. Pediatr Dent. 2000 May-Jun;22(3):232-3.
- Chaparro-Avendano AV, Berini-Aytes L, Gay-Escoda C. Peripheral giant cell granuloma. A report of five cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2005 Jan-Feb;10(1):53-7; 48-52.
- Neville BW, Damm DD, Allen CM, Bouquot JE. Peripheral giant cell granuloma. In: Oral and Maxillofacial Pathology, 2nd edition. Philadelphia: W.B. Saunders, 2002. p. 449-451.
- Hanemann JA, Pereira AA, Ribeiro Junior NV, Oliveira DT. Peripheral ossifying fibroma in a child: report of case. J Clin Pediatr Dent. 2003 Spring;27(3):283-5.
- Walters JD, Will JK, Hatfield RD, Cacchillo DA, Raabe DA. Excision and repair of the peripheral ossifying fibroma: a report of 3 cases. J Periodontol. 2001 Jul;72(7):939-44.
- Cuisia ZE, Brannon RB. Peripheral ossifying fibroma–a clinical evaluation of 134 pediatric cases. Pediatr Dent. 2001 May-Jun;23(3):245-8
Sorry! you are incorrect
Peripheral ossifying fibroma constitutes 10% of all reactive gingival swellings. It consists of a moderately cellular fibrous connective tissue mass with bony trabeculae and/or cementum-like hard tissue. It has been reported but rarely on edentulous alveolar mucosa. It originates from the periodontal ligament or the periosteum. This lesion is most common in young patients between 1 and 19 years of age and has a predilection for females over males by a 3:2 ratio (7-9). It occurs exclusively on the gingiva, especially the anterior gingiva, with slight predilection to the maxilla and rare presentation in primary teeth (9). It is usually sessile and exophytic and often ulcerated; it presents as well-demarcated sessile nodules, which are firm or hard depending on the amount of ossification and calcifications (7-9). Peripheral ossifying fibroma is usually pink but can be focally red if ulcerated. Histologically, peripheral ossifying fibroma is made up of a moderately cellular mass of fibrous connective tissue with calcifications ranging from cementum-like material to calcified bony trabeculae with viable osteocytes. The surface epithelium overlying the mass is usually ulcerated. Deep surgical excision to include the periodontal ligament is the preferred treatment, though laser removal has been used effectively. Deep surgery may lead to a gingival defect, which would require gingival grafting, especially if it is located on the anterior buccal gingival (9). There is a 16-20% recurrence rate (9).