Left mandible, lingual-exophytic radiopaque lesion
Contributed by Drs. Srinivasa R. Chandra & Randy Eggert
Harborview Medical Center & Redmond Oral & Maxillofacial Surgery, WA
Case Summary and Diagnostic Information
This is a 28-year-old Caucasian male who presented with an exophytic lingual plate expansion in the left posterior mandible.
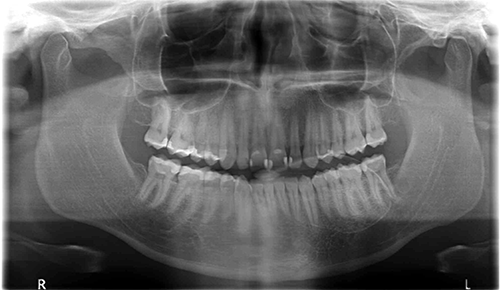
This is a 28-year-old Caucasian male who presented with an exophytic lingual plate expansion in the left posterior mandible (Figure 1). The panoramic radiograph demonstrates a well-defined exophytic radiopaque lesion protruding into the floor of mouth and measuring approximately 4 X 2 cm. The lesion had grown gradually since the patient was 13 to 16 years of age, and has not been accompanied by pain or bleeding. The associated teeth are vital. The lesion was surgically removed, and recurred within a year (Figure 2).
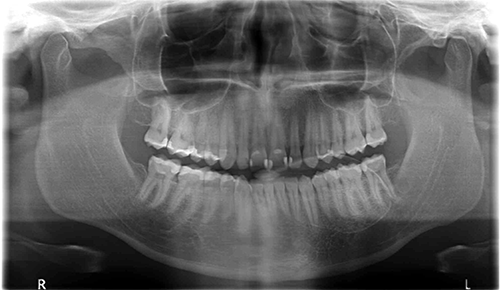
Figure 1 This is a panoramic radiograph taken at the first presentation, demonstrating a large radiopaque lesion in the left posterior mandible projecting as a well demarcated radiopaque lesion.

Figure 2 This is a radiographic image of the recurrence, demonstrating a cone bean CT image of a well-demarcated exophytic radiopaque lesion protruding into the floor of mouth from the body of the left mandible.
The patient denied any past medical history or history of trauma.
The patient presented with a single exophytic bony lesion involving the lingual posterior left mandible. The area was firm and non-tender to palpation. No trismus, bruit, or sensory deficits were elicited. The primary lesion, which had increased in size over a 12 to 15 year period, occupied the left floor of the mouth. It was conservatively excised by Dr. Eggert, and recurred within a year of removal. The recurrence was removed by Dr. Chandra. The primary lesion is depicted in Figure 1 and the recurrence in figures 2 and 3.

Figure 3 This is a clinical image of the recurring lesion taken at surgery after the flap was raised. It shows the mandibular lingual bony protrusion into the floor of the mouth.
The patient underwent conservative excisional removal, during which extensive hemorrhage was encountered. Eight to twelve months following excision, the lesion recurred. A CT contrasted angiogram was performed with interventional radiology. Vascular perfusion was identified and the second surgical resection was performed under conditions of good vascular access and control of external carotid artery feeders. When seen six months following resection of the recurrent lesion, the patient was asymptomatic in the affected region.
Histologic examination revealed a large, decalcified and multisected nodule of hard and soft tissue embedded in multiple blocks. All the fragments displayed similar morphology of a bony nodule containing a lesion of vascular origin (Figures 4 & 5). The bony nodule was made up of lamellar viable bony trabeculae surrounding spaces filled with a lesion of vascular origin. The latter was made up of spaces of variable shapes and sizes lined by one layer of flat endothelial cells and filled with erythrocytes.
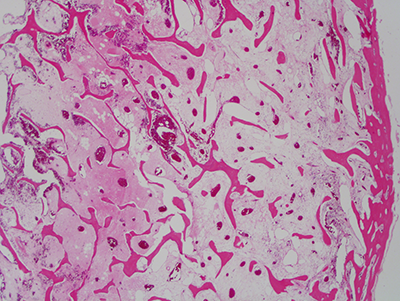
Figure 4 This is a low power (40X) micrograph of an H & E stained section, representing a decalcified fragment of bone made up of a lesion of vascular origin surrounded by delicate fibrous connective tissue, aggregates of fatty marrow, and bony trabeculae mostly lamellar in type. The lesion of vascular origin is made up of many vascular spaces, of variable shapes and sizes, lined by one layer of flat endothelial cells and mostly filled with erythrocytes.
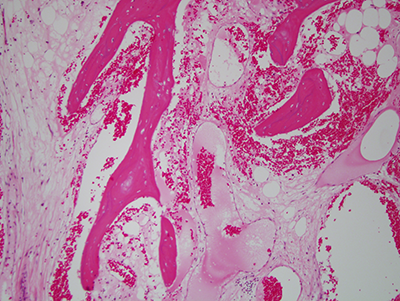
Figure 5 This is a higher power (100X) micrograph of an H & E stained section demonstrating the large vascular spaces at a close level. These spaces are lined by one layer of flat endothelial cells.
After you have finished reviewing the available diagnostic information