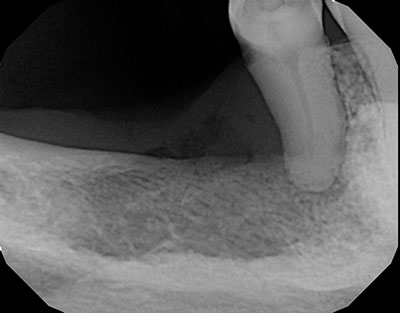
Expansile, radiopaque/radiolucent lesion, right posterior mandible
Can you make the correct diagnosis?
The patient is a 67-year-old female who presented with diffuse pain in the right posterior mandible in edentulous area of tooth #29 affecting tooth #29.
Sorry, you are incorrect!
The clinical presentation of pain and discomfort in an edentulous area associated with mobile tooth #29 when combined with the radiographic finding of predominantly radiopaque lesion is consistent with the clinical and radiographic presentation of chronic sclerosing osteomyelitis; thus, it would be a reasonable condition to include on the differential diagnosis. However, the histology of this specimen was not supportive of osteomyelitis.
Chronic sclerosing osteomyelitis is a challenging condition to diagnose both clinically and histologically. This condition has gone by a series of names, starting with “ossifying osteomyelitis”, a term used by Thoma in the 1940s. The current name was first used by Shafer in 1957 where he divided the histopathological patterns into “focal” and “diffuse” subtypes. This condition is most commonly found in the mandible, is more prevalent in females, and usually presents with pain and local swelling with periodic exacerbations. Most investigators agree that this type of osteomyelitis is not usually associated with suppuration or fistula formation. Some reports indicate that mild suppuration may develop, but this occurs rarely.
Chronic sclerosing osteomyelitis can occur at any age, including in children under the age of ten. The type that occurs in children is called “juvenile mandibular chronic osteomyelitis” which affects 6-12 year old children, mostly girls; it occurs mainly in the mandible. The adult type affects people 30-40 years of age, and is twice as common in females but shows no race predilection. It too is by far more common in the mandible, especially the posterior mandible, as is the case in this patient. Patients present with a history of years of pain with episodic exacerbations. Some investigators have been successful in isolating E corrodens from the lesions, while most have not been able to grow any micro-organisms. Radiographically, chronic sclerosing osteomyelitis presents as diffuse, irregular aggregates of bone with indistinct borders. It may mimic Paget’s disease. Histologically, the biopsy shows dense bone with a “mosaic” consistent with a reactive process. The surrounding soft tissue may contain neutrophils during the acute stage, and variable number of chronic inflammatory cells, mainly lymphocytes and plasma cells. It is a challenge to treat chronic sclerosing osteomyelitis. Antibiotics, especially penicillin and doxycycline, and decortications seem to be effective at the early stages may help prevent the disease from progression. Resection has occasionally and in rare cases, been used. The literature indicates that NSAIDS are useful in controlling the intensifying pain. Hyperbaric oxygen is reported to be effective in some cases.
Sorry, you are incorrect!
The predominant radiopaque radiographic appearance with orange-peel morphology should make one think of two potential conditions and those are “fibrous dysplasia (FD)” and primary “hyperparathyroidism.”
Regarding FD, this patient is too old and the lesion is in the mandible, both argue against FD and should not be seriously considered on the DDX in this case.
As to hyperparathyroidism, the age and gender as well the site are all consistent with this condition. The radiographic changes are also consistent with this condition. The histology however is not consistent with hyperparathyroidism.
Hyperparathyroidism is the result of excessive production of parathyroid hormone (PTH) needed for calcium release. PTH stimulates the osteoclasts to resorb bone and release calcium unto the blood stream. When too much PTH is present, there will be generalized bone resorption but more so in the small bones such as the jaws and the small finger bones. There are two types of hyperparathyroidism: primary and secondary: primary is the type that applies to this case. Primary hyperparathyroidism is associated with parathyroid adenoma, but possibly parathyroid hyperplasia and rarely adenocarcinoma. Secondary is usually associated with chronic renal disease (renal osteodystrophy) where ions such as calcium are lost through renal failure and demand for calcium production comes as a secondary factor. This patient has normal kidney functions.
Primary hyperparathyroidism is three times more common in females is more common in middle age females. It may produce multiple bone lesions known as ‘brown tumor’ because of the chocolate color of the soft tissue within the bone. Stones, bones, moans and groans are clinical characteristic associated with this condition. Laboratory tests show increased levels of PTH. Hypercalcemia may be present which may be accompanied by hypophosphatemia. Radiographically is associated with loss of density which can range from irregular radiolucent lesions that may be multiple or may have a ‘ground-glass’ appearance which is close to the radiographic changes in this patient. Medical and/or surgical management of the underlying condition (i.e. surgical removal of the adenoma in primary and renal transplant in secondary) results in resolution.
Congratulations, you are correct!
The age of this patient is consistent with oral SCC while the gender is not. This patient has history of cigarette smoking but not currently. The site is also not typical since gingival SCC constitutes the third most common site for oral SCC after lateral/ventral tongue and floor of mouth. The clinical presentation of loss of periodontal support and extraction of tooth #29 are all features that should make one want to rule out SCC. The radiographic features of orange peel are also not typical of the bony involvement of gingival SCC. About one-half of gingival SCC invade bone; they are usually radiolucent and grow vertically in a “funnel- shaped” appearance. The histology is that of SCC of the gingiva.
Gingival and alveolar ridge SCC accounts for 10-12% of all oral carcinomas. The mandibular gingiva is affected more commonly. It is more common in heavy cigarette smokers and presents as a non-healing ulcer, severe localized periodontitis or an exophytic lesion. Bone invasion is common (50%) and is usually radiolucent.
Sorry, you are incorrect!
The site and clinical presentation of pain are consistent with metastatic disease to the jaw. However, since cancer metastasis to the oral cavity is so rare (less than 1% of all oral malignancies), it would be highly unlikely to be metastatic disease. The radiographic appearance of predominantly radiopaque lesion, also argues against metastasis especially in a female patient. Over 90% of cancer metastasis cases are radiolucent. In males however, prostate cancer can produce radiopaque lesion in the jaw on metastasis. The histology is not consistent with cancer metastasis.
Cancer metastasis to the oral cavity is neither specific nor common. Although it constitutes less than 1% of all oral malignant neoplasms, it may have devastating implications for the patient, mainly because metastasis to other sites has already developed or is inevitable. Theoretically, any malignant neoplasm can metastasize to the oral cavity, but in actuality few do and out of the ones that do, the majority are carcinomas rather than sarcomas. The malignant neoplasms that metastasize most commonly to the mouth are primary cancers of the breast, lung, kidney and prostate. The only cancer that commonly produces bone-containing metastases in the jaws is prostate cancer, although occasionally breast cancer can produce bone as well.
Breast cancer metastasis to the jaws is the most common followed by lung and prostate, colon, kidney and others. By far the most common location for cancer metastasis to the mouth is the posterior mandible, where 80% of cases occur, followed by the gingiva. The maxilla is a rare location for tumor metastasis, described mainly in adults over the age of 30 and rarely in children. Pain and swelling are the most common clinical symptoms.