Expansible multilocular radiolucency: Left posterior mandible
Can you make the correct diagnosis?
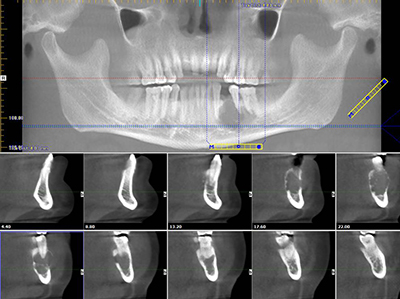
This is a 50-year-old Hispanic male who presented with a lesion of less than a year’s duration in the posterior mandible.
Solid Ameloblastoma with mixed histologic subtypes
Differential Diagnosis
- Malignant neoplasm of the jaw
- Metastatic
- Primary ie. malignant lymphoma, osteosarcoma, chondrosarcoma
- Odontogenic neoplasm
- Solid ameloblastoma
- Odontogenic myxoma
- CGCG
Sorry, you are incorrect!
The patient’s numbness in the chin and lower lip, 15-pound weight loss, and localized gross tooth mobility are all symptoms that can be consistent with metastatic diseases to the jaw. The patient’s type of anesthesia, known as “numb chin syndrome,” is usually associated with metastatic disease to the posterior mandible where the neoplastic cells invade the alveolar or mental nerve. Cancer metastasis to the mouth is very rare and is a random process. The most common presentation of cancer metastasis to the mouth is radiolucency in the posterior mandible associated with pain, numbness, or both, as noted in this patient. However, this patient’s multilocular configuration is not consistent with malignant behavior. While primary or metastatic malignant neoplasms of the jaw may rarely have well-demarcated margins in early stages, this behavior is highly unusual. For that reason, the well-demarcated margins, in this author’s opinion, make a malignant neoplasm unlikely.
In summary, the posterior mandible radiolucency, the numb chin and lip, the loss of 15 pounds, and the 3+ tooth mobility combined with the age of the patient are all factors indicating that metastatic disease should be seriously considered. The patient’s lack of a history of a malignant neoplasm elsewhere should not prevent the inclusion of metastasis on the differential diagnosis since, in rare cases, an oral manifestation can be the first sign of a silent primary malignancy. In this case, metastasis was ruled out based on clear histological features indicating a primary neoplasm.
Sorry, you are incorrect!
The patient’s chin and lower lip numbness, 15-pound weight loss, and localized gross tooth mobility are all symptoms that usually indicate malignancy in the jaw, whether metastatic or primary. The primary malignancies of the mandible that are known to be associated with such symptoms include primary malignant lymphoma of bone, osteosarcoma and chondrosarcoma.
Peripheral blood malignant neoplasms are usually completely radiolucent and can occur in the jawbones, especially in the posterior mandible. The age, gender, weight loss and localized gross tooth mobility are consistent with that of primary malignant lymphoma of bone; 92% of cases occur in patients over the age of 30, the majority over the age of 60. Primary malignant lymphoma of bone is slightly more common in males.
The posterior mandible is also a common location for osteosarcoma, which is the most common bone malignancy. However, osteosarcomas are usually ill-defined and are mixed radiolucent/radiopaque lesions. They can be completely radiolucent, but this is exceedingly rare. Osteosarcomas of the jaw have an average age of occurrence of 33 years, so this patient is on the older age for osteosarcoma. The patient’s gender is supportive of this diagnosis; it is slightly more common in males.
The age and gender are consistent with chondrosarcoma, but the site is not, since chondrosarcomas of the jaw tend to occur more often in the maxilla than in the body of the mandible. Like osteosarcomas, the radiographic presentation of chondrosarcomas is usually ill-defined and is also usually mixed radiolucent and radiopaque.
Again, the radiographic findings of multilocular radiolucency and well-demarcated margins argue against this lesion being malignant, whether a primary malignancy of the jaw or metastatic disease to the jaw. The histology is not supportive of malignant lymphoma of bone, osteosarcoma, or chondrosarcoma.
Congratulations, you are correct!
The location in the posterior mandible and the radiographic findings of a well-demarcated, multilocular and expansile radiolucency are all consistent with solid ameloblastoma. Perforation of the jawbone and localized tooth mobility area also consistent with the known behavior of benign but locally aggressive solid ameloblastoma. Pain is unusual with ameloblastomas, but if inflamed, any odontogenic or nonodontogenic neoplasms of the jaws can be painful. The lower lip and chin numbness is very rare in association with ameloblastomas, but it has been described, especially in larger tumors that can push on the alveolar nerve and cause numbness. The age of the patient is on the older end of the typical range; the average age of occurrence for solid ameloblastoma is 33 years. Although it is well reported that ameloblastomas are not gender specific, there are reports that indicates them to be slightly more prevalent in males with a male-to-female occurrence ratio of 1.1-1.7:1. The histology in this case is supportive of solid ameloblastoma.
Sorry, you are incorrect!
The location, the multilocular radiolucency, the expansion, and the well-demarcated radiographic morphology are all consistent with the behavior of a benign neoplasm, including that of an odontogenic myxoma. The perforation of jawbone and tooth mobility are unusual with odontogenic myxomas but are known to happen, since they too are benign but locally aggressive tumors. The known age range of occurrence is 23-30 years, and it rarely occurs over the age of fifty, so this patient is somewhat old for this diagnosis. The numb chin and lower lip are not reported in odontogenic myxomas. The histology is not supportive of odontogenic myxoma.
Sorry, you are incorrect!
The site of occurrence anterior to the first molar and the radiographic presentation of a well-demarcated and expansile multilocular radiolucency are consistent with the clinical behavior of central giant cell granuloma (CGCG). Over 70% of CGCG cases occur anterior to the first molar. Perforation of bone and tooth mobility, although unusual, are sometimes reported in association with CGCG. The age and gender of this patient, however, are not consistent with CGCG. Over 60% of CGCG cases occur in patients younger than 30 years of age, with twice as many occurrences in females as in males. The numb chin and lower lip are not reported in CGCG. The histology is not supportive of CGCG.