All cases are discussed by: Dr. Dolphine Oda, UW-Oral Pathology Biopsy Service
Unilocular radiolucency between teeth #s 26 & 27
Contributed by: Dr. Adrian Pawlowski
Bell Harbor Dental, PerioInnovation, Seattle WA
Case Summary and Diagnostic Information
This is a 66-year-old male who presented for diagnosis and treatment of a radiolucent lesion between #s 26-27 (Figures 1-2).
This is a 66-year-old male who presented for diagnosis and treatment of a radiolucent lesion between #s 26-27 (Figures 1-2). Three weeks prior, he experienced pressure building up in his jaw bone/gum in area buccal to teeth #26-27 (Figure 2). Uniquely, the patient had had a similar lesion removed in 1996 between teeth #s 28-29. This information was collected from features of a periapical radiograph (Figure 3), pathology report, and surgery notes from that time.
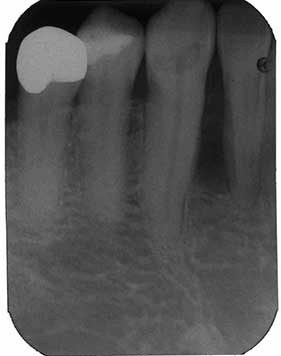
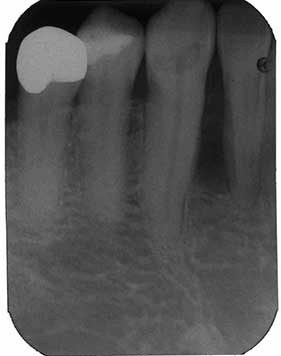
Figure 1 2018: This is a periapical radiograph taken by the general dentist at the first clinical presentation. Note a well-demarcated unilocular radiolucency between teeth #s 26-27 involving the full-length of the roots. It is mildly pushing teeth apart. There is no evidence of tooth resorption.
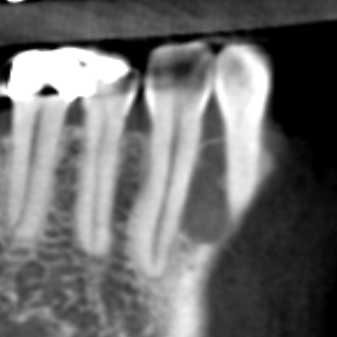
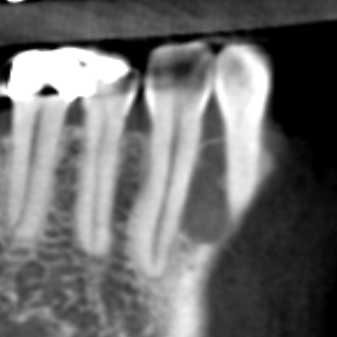
Figure 2 2018: This is a section of a cone beam CT radiograph taken by the periodontologist prior to treatment. This radiograph clearly shows a well-demarcated unilocular radiolucency between teeth #s 26-27 mildly pushing teeth apart. There is no evidence of tooth resorption.

Figure 3 1996: This is a periapical radiograph taken in 1996 at first clinical presentation. Note a smaller and well-demarcated unilocular radiolucency between teeth #s 28-29 at the superior/slightly middle length of the roots. It is not pushing teeth apart and is not causing tooth resorption.
The past medical history is significant for malignant melanoma and hypothyroidism. The malignant melanoma was treated with surgical excision a few years ago. The patient is a nonsmoker. He reports allergies to latex and amoxicillin.
The clinical history shows that, in 1996, this patient had a lesion conservatively curetted from the area between teeth #s 28-29 (Figure 3). The area healed with no complications. In 2018, a new larger lesion resembling the original lesion was identified between teeth #s 26-27, slightly anterior to the lesion from 1996. At this point, it is difficult to definitively determine if the current lesion is a recurrence or a second primary occurrence. Since the histology and clinical presentation of the current lesion is very similar to that of the 1996 lesion, the reviewer considers the current lesion to be more consistent with a recurrence. This perspective will be discussed in the differential diagnosis portion of this case.
The procedure was performed under local anesthesia; a sulcular incision was made from the anterior mandible in order to expose the buccal bone. There was no buccal cortical bone and the lesion was found to semi-solid to cystic in consistency. It was not fluid filled. The lesion was adherent to the bony cavity and required considerable scraping to detach it. Though it appeared to be a smooth-walled teardrop-shaped radiolucent lesion on the periapical radiograph, at surgery there appeared to be at least 3 compartments with the appearance of soap bubbles in the coronal and lingual aspect of the lesion. The lesion was enucleated and the surgical site was thoroughly irrigated and closed. A 10-day postoperative visit demonstrated loosening of tooth #26 as well as tenderness. No drainage or numbness was noted.
The histology of the current specimen is very similar to that of the 1996 biopsy. The specimen is cystic, covered by epithelium of variable thickness focally forming epithelial spherules (Figures 4-6). In some areas, the epithelium shows changes in the basal and para-basal cell layers (Figures 5-6). The basal cell layer is columnar and palisaded with hyperchromatic nuclei. It is polarized in focal areas. Spindle-shaped epithelial cells simulating stellate reticulum are present but rare. The connective tissue ranges from lose and cellular to fibrotic. One epithelial island with palisaded and polarized columnar cells at the periphery is identified in the connective tissue wall (Figure 6).
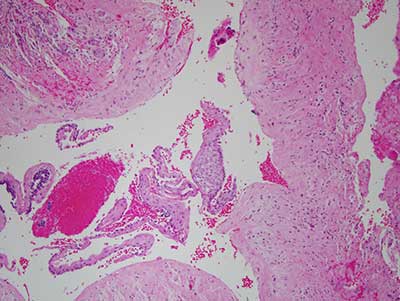
Figure 4 This is an H & E stained section at x 100 magnification demonstrating a cystic structure lined by non-keratinized epithelium of variable thickness focally forming epithelial spherules; one is identified in this figure.

Figure 5 This is an H & E stained section at x 100 magnification demonstrating a cystic structure lined by epithelium with basal cell layer that is low columnar to cuboidal and is palisaded with hyperchromatic nuclei. The nuclei are focally polarized. The connective tissue ranges from lose and cellular to fibrotic.
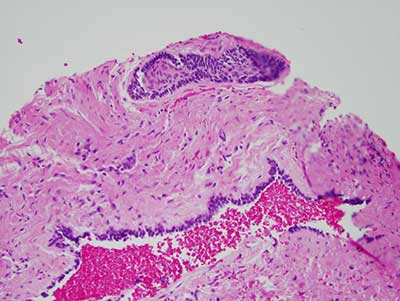
Figure 6 This is an H & E stained section at x 100 magnification demonstrating a cystic structure lined by epithelium with basal cell layer that is columnar and palisaded with hyperchromatic nuclei. The connective tissue wall contains one epithelial island with palisaded and polarized columnar cells at the periphery. The center of the island contains stellate reticulum-type of epithelial cells.
After you have finished reviewing the available diagnostic information