Ill-Defined Radiolucency; Left Posterior Mandible and Ramus
Can you make the correct diagnosis?
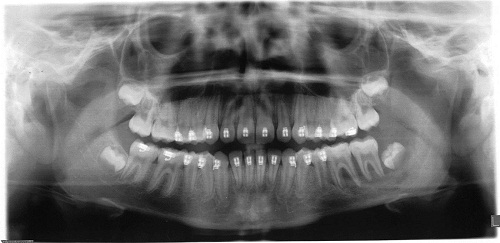
This is a 13-year-old white male who presented for an emergency exam of a large swelling in the left posterior mandible and ramus area.
Sorry! you are incorrect
The age of the patient, the soft tissue mass, the fast growth, and the destructive nature of the lesion are all in support of a condition that is aggressive in behavior. However, it is difficult to tell if the lesion is an aggressive soft-tissue neoplasm that is invading the bone or if this is an aggressive bone neoplasm perforating it and forming a soft tissue mass. The age and gender of this patient, the location, the soft tissue mass and the bony destruction are all supportive of aggressive fibromatosis but the histology is not.
Aggressive fibromatosis represents a group of fibrous neoplasms with various clinical behaviors and histologic presentations. Aggressive fibromatosis is known by many names, including juvenile aggressive fibromatosis, infantile desmoid fibromatosis, and nonmetastasizing fibrosarcoma. The last nomenclature best describes the behavior of this lesion; it is a benign but locally infiltrative and aggressive neoplasm with a potential for multiple local recurrences, but no potential for metastasis. Aggressive fibromatosis can be sporadic or familial, such as those associated with Gardner’s syndrome. The latter tends to occur more in the abdominal area, and rarely in the head and neck area. Some investigators consider aggressive fibromatosis in children to be a separate entity than that which occurs in adults.
Head-and-neck aggressive fibromatosis usually occurs in children under 20 years of age. Among adults, it is more prevalent in females by a ratio of 2:1; in children, it occurs more often in males by a ratio of 2:1. It typically presents as a firm, painless, rapidly growing asymptomatic mass. Occasionally, it is slow-growing, but it is destructive in either case. It can destroy bone, infiltrate adjacent structures, displace teeth, and induce periosteal reaction, rendering it clinically and radiographically difficult to differentiate from a sarcoma. It presents in multiple locations within the oral cavity, including the gingiva, lips and other oral soft tissue areas. Several theories have been proposed regarding the etiology of aggressive fibromatosis, which is currently unknown. Hormonal, viral, chromosomal, and, occasionally, trauma-induced etiologies have all been described. Trauma-induced etiology is often described in the area of caesarean-section scars. There is a legitimate body of evidence to suggest that estrogen promotes the growth of fibromatosis, particularly in pregnant females. Association with the FAP (Gardner’s Syndrome) gene is also well documented. The clinical behavior of aggressive fibromatosis is unpredictable and ranges from frequently recurring to spontaneously regressing; for that reason, a variety of treatment modalities have been employed. Surgery, which is the treatment of choice, ranges from complete removal with clean margins to debulking of the lesion to avoid loss of vital structures. The latter method is often necessary for oral cavity lesions. In the present case, care was taken during surgery to avoid sacrificing the lingual nerve; therefore, the surgeons opted for the more conservative approach of debulking of the primary lesion and very close watch of the surgical area. Several non-surgical alternative treatments have also emerged, such as radiotherapy, chemotherapy, hormonal and biological manipulation, and non-steroidal anti-inflammatory agents. Surgery combined with radiotherapy or chemotherapy has been used in recurring and persistent lesions. Radiotherapy is a secondary treatment method to surgery, and is sometimes used alone. However, concern over its possible adverse long-term effects, especially in children, makes it a less desirable mode of therapy. Chemotherapy, with single or multiple agents, and neoadjuvant or maintenance therapy have also been used. In children, chemotherapy is associated with long-term adverse effects and occasional serious complications and even death. Some cases have been successfully treated with alternative treatments such as estrogen antagonists and non-steroidal anti-inflammatory drugs. Prognosis and recurrences are difficult to predict. The recurrence rate ranges from 20% to 70% for aggressive fibromatosis in children, and most recurrences occur within the first five years. Some studies suggest that positive margins may be the only predictor for recurrence, if any. Other adverse prognostic factors may include an age of less than 18 years, recurrent disease, and surgical treatment alone.
Congratulations! You are correct
Langerhans cells are dendritic cells of bone-marrow origin. Langerhans cell histiocytosis is generally a disease of children and rarely affects adults. The old name for this condition is histiocytosis X, and it was classified into several types: eosinophilic granuloma (monostotic and polyostotic), Hand-Schuller-Christian disease, and Letterer-Siwe disease. The first two types (EG and HSC) were considered less aggressive and chronic in clinical behavior while the last (LS) was more aggressive and acute in behavior. Currently, the classification system for this disease divides patients into unifocal, multifocal/unisystem and multifocal/multisystem types. This classification also divides patients into low- and high-risk categories; patients with the former two types of the disease are considered low risk, while those with the latter type are considered high risk. The disease is low risk if it affects one organ, whether in one site or multiple sites within that organ (e.g. bone, lymph nodes, skin or pituitary gland). If the disease involves multiple organs such as the lungs, liver, spleen and bone marrow (multifocal and multisystem), it is considered to be of the high-risk type.
Langerhans cells are CD1a positive; for that reason, immunohistochemistry staining is very helpful. They are also S-100 and CD45 positive. Langerhans cells can also be comfortably identified by the H & E stain. LCH usually presents with pain and swelling but can also be asymptomatic. The bony lesions are usually aggressively lytic, especially those of the mandible. As mentioned above, this disease rarely occurs in adults and that more than 50% of the cases affect children under 10 years of age, with a male predilection.
Adult LCH most commonly affects the bones, especially the jaws and skull bones in general. LCH of the jaw bone usually presents as either localized severe periodontitis or generalized severe periodontitis. It can also affect the skin, lymph nodes, and less commonly the pituitary glands and lungs. Radiographically, the bony lesions are sharply radiolucent and the jaw lesions give the impression of teeth “floating” in space due to the significant bone destruction. Treatment includes curettage, especially of the jaw lesions. Chemotherapy and low-level radiotherapy have also been effective. The unifocal disease has an overall 95% survival rate. Cases with two-organ involvement have a 75% overall survival rate. The more organs are involved, the less favorable the prognosis.
Sorry! you are incorrect
The fast growth, the location, the destructive nature of the lesion, and the age and gender of the patient are all supportive of a diagnosis of Burkitt’s lymphoma; for that reason, it should be on the differential diagnosis. The histology, however, is not supportive of BL.
Burkitt’s lymphoma (BL), also known as African Jaw Lymphoma, was first described in children of Kampala, Uganda. This lesion is also described outside Africa, including in the U.S.A. Burkitt’s lymphoma is classified into three types: Endemic (African); Sporadic (Non-endemic); and Immunodeficiency-associated. The sporadic form of BL is most commonly described in the United States. Burkitt’s lymphoma presents clinically as a rapidly-growing tumor mass and is more common in the maxilla than the mandible. It is also more common in males by a ratio of 3:1 with an age range of 10-12 years of age. The endemic African type is a very rapidly growing and destructive lesion that occurs as a jaw neoplasm in up to 70% of cases. Its location is usually in the maxilla, but sometimes all four quadrants are involved. The average age of patients with this condition is 7 years. These patients have elevated titer to Epstein Barr Virus (EBV). The Sporadic type generally involves lymph nodes, lymphoid tissue, and/or visceral organs, especially the abdomen. Jaw involvement is reported but uncommon. These patients occasionally demonstrate EBV antigen titers.
Sorry! you are incorrect
The destructive nature of this lesion, the age and gender of the patient, and the location are all consistent with the behavior of Ewing’s sarcoma; for that reason, it should be on the differential diagnosis. The histology, however, is not supportive of ES.
Ewing sarcoma is a malignant neoplasm primarily of bone constituting 6-8% of primary bone malignancies. It is the third most common such neoplasm generally speaking after osteosarcoma and chondrosarcoma. It is of unknown histogenesis, but immunohistochemistry stains of this neoplasm suggest that the cells are of neural crest origin. Extraskeletal (soft tissue) Ewing’s sarcoma is also described, but not commonly. Up to 90% of these cases show reciprocal translocation between chromosomes 11 and 22. Clinically, this neoplasm usually presents with pain and swelling of a short duration. Soft-tissue swelling overlying the bone is often present because the tumor perforates the bone in a soft-tissue mass. The most common bones affected by this neoplasm are the long bones, pelvis and ribs; the jaw bones are much less commonly affected, and of the two, the mandible is more commonly affected than the maxilla. It has a slight predilection for occurrence in males and has a peak incidence in children 10 to 15 years old. It is by far more common in Caucasians and is very rare in blacks and Asians. Radiographically, it usually presents as an ill-defined radiolucency with a moth-eaten appearance in some cases. The typical onionskin reaction of the periosteal reaction is common in the long bones and less common in the jaw bones. Histologically, it is characterized by sheets of round blue cells with hyperchromatic nuclei and clear cytoplasm. Immunohistochemistry staining demonstrates the presence of the cell surface antigen CD99, but other neoplasms also express this marker.