Return to Case of the Month Archives
February 2009: Dark brown to black gingival swelling, right posterior palate
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Contributed by
Dr. Brian C. Rubens
Surgery of the Facial Skeleton, Jaws & Teeth, Bothell, WA
Case Summary and Diagnostic Information

This is an 82-year-old white female whose chief complaint was a painful lesion in the right posterior palate associated with the palatal gingiva of tooth # 2 (Figure 1).
Diagnostic Information Available
This is an 82-year-old white female whose chief complaint was a painful lesion in the right posterior palate associated with the palatal gingiva of tooth # 2 (Figure 1). The patient stated that the lesion was painful and that “it feels like it festers.” The lesion had a distinct rolled border with a crater that was focally ulcerated. The lesion was not uniform in color. It had a spectrum of discoloration ranging from tan spots away from the rolled border to brown and deep brown, almost black, around the rolled border. It was of six weeks’ duration.

Figure 1 Clinical photograph of the lesion taken at the first visit. Note the rolled border with central concavity and focal ulceration. Also note the range of discoloration from tan to deep brown
The patient’s past medical history is significant for atrial fibrillation and asthma. She had a thyroidectomy as a teenager, an appendectomy in 1948 and a hysterectomy in 1976.
In September 2008 the patient noticed a small “bump” in her posterior right palate. This did not cause her any difficulties with swallowing, speech or numbness. The swelling slowly increased in size. In mid October the lesion became progressively larger and darker at the periphery. The center was concave with an ulcerated or granulomatous look and the periphery was rolled. It was painful but still did not interfere with swallowing or speech.
Treatment
The lesion was biopsied under local anesthesia. The results of the incisional biopsy led to a referral to an ENT surgeon for further treatment. In November of 2008 she underwent a right partial maxillectomy. Since her surgery she has lost approximately 10 pounds, primarily due to difficulty with swallowing. However, her swallowing has since improved.
Incisional and excisional biopsy
Histologic examination of the H & E section revealed numerous atypical melanocytes with varying degrees of cellular and nuclear pleomorphism and large nuclei with prominent nucleoli (Figures 2 & 3). The atypical melanocytes involved most of the superficial epithelium and also invaded the superficial lamina propria (Figures 2 & 3). The depth of invasion of the incisional biopsy was 1.1 mm while that of the surgical specimen was 4 mm. The neoplastic cells were actively producing and releasing melanin pigment. The immunohistochemistry stain was uniformly positive with Melan-A (Figure 4) and with S-100 antibodies (Figure 5).
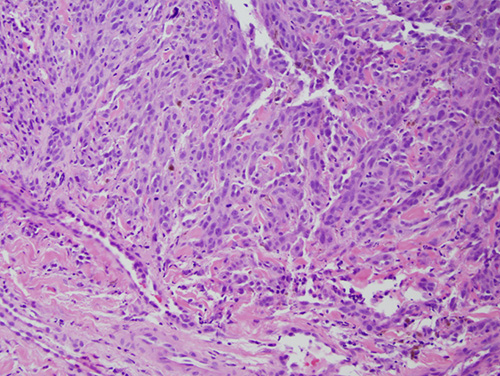
Figure 2 Low power (x100) histology shows H & E stained section with surface epithelium exhibiting atypical melanocytes with varying degrees of cellular and nuclear pleomorphism and large nuclei with prominent nucleoli. The cells invade the superficial lamina propria by 1.1 mm.
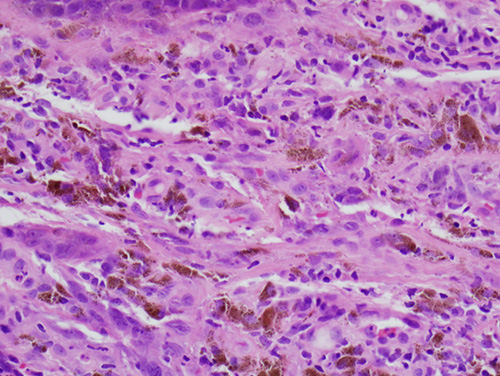
Figure 3 Higher power (x200) histology shows the atypical melanocytes high within the surface epithelium as well as invading the superficial lamina propria. Note the amount of melanin produced by these cells.
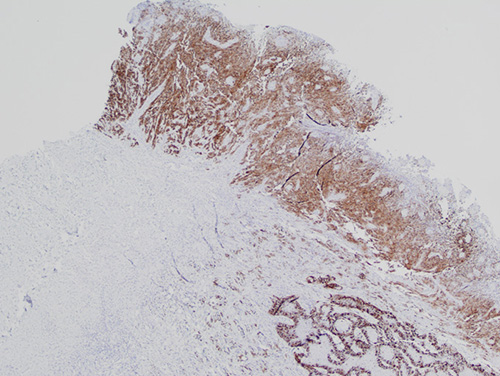
Figure 4 Low power (x40) Immunohistochemistry stain with Melan A antibody. Note the uniform positive epithelial staining most in the surface epithelium but some in the superficial connective tissue.
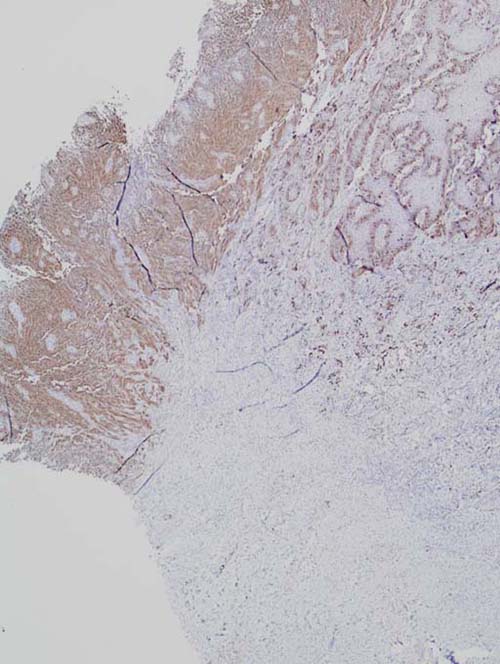
Figure 5 Low power (x40) Immunohistochemistry stain with S-100 protein. Note the uniform positive epithelial staining most in the surface epithelium but some in the superficial connective tissue.
After you have finished reviewing the available diagnostic information