Single Large Swelling Right Posterior Maxillary Vestibule and Buccal Mucosa
Can you make the correct diagnosis?
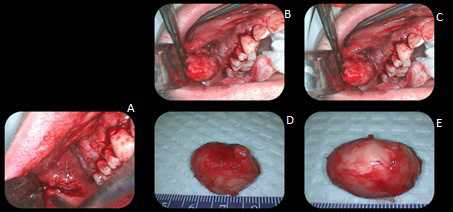
This is a 47-year-old male who presented with a large, firm mass that was mobile within his cheek.
Sorry! you are incorrect
The age of the patient, the slow growth of the lesion, and the clinical description of being asymptomatic are all consistent with a diagnosis of lipoma. The gender of the patient may also be consistent depending on whose report one reads. The gross morphology of an encapsulated yellow-tan nodule is supportive of a lipoma. The location in the posterior vestibule, however, is rare for a lipoma. The histology is not consistent with a lipoma.
Lipomas are benign neoplasms of adipose tissue origin. They are more commonly described in the trunk and extremities and are rare in the oral cavity. Their overall incidence in the oral cavity accounts for around 4.4% of all benign oral lesions. In a recent study from the Armed Forces Institute of Pathology (AFIP) of 125 benign lipomas in and around the mouth, the male to female ratio was approximately 3:1, which is not surprising given that the study was conducted within a military population. Other studies reveal an equal gender distribution. The AFIP study showed the mean age to be 52 with a range of 9-92 years. Only 4 of the 125 cases involved patients less than 18 years of age. In the mouth, the most common location for this neoplasm is the buccal mucosa, followed by the lips, submandibular area, tongue, palate and, less often, the floor of mouth and vestibule. These findings are consistent with many other published reports. These lesions are slow growing and can be present for many years. Lipomatous nodule of the buccal mucosa may represent herniation of the buccal fat pad. Lipomas usually present as a single, smooth surfaced, soft with doughy consistency, lobulated, painless, yellowish, sessile nodule. The overlying mucosa is usually thin and stretched with visible blood vessels. Because of its softness it can be mistaken for a cyst. Histologically, lipomas are variable benign histologies. Some have predominant lobules of mature adipocytes surrounded by a thin connective tissue capsule, while others have a predominant spindle-cell component, myxoid, chondroid, or connective tissue component. Some are intramuscular. Each has its own clinical behavior. Simple surgical excision is the treatment of choice for the simple, mature adipocyte component.
Congratulations! You are correct
A long-standing nodule in the buccal mucosa should make a clinician think of benign salivary gland neoplasms, the most common of which is pleomorphic adenoma (PA). The age of this patient is typical, but not the gender. The location is also not typical of PA. The gross morphology of an encapsulated yellowish-tan nodule is consistent with a PA, and the histology is that of PA.
Pleomorphic adenoma is the most common benign salivary-gland neoplasm of both the major and minor salivary glands. It originates from the myoepithelial cells and the reserve cells of the intercalated ducts. It accounts for 80% of all benign salivary gland neoplasms. It occurs in both major and minor salivary glands and accounts for up to 77% of parotid, 68% of submandibular, and 43% of minor salivary gland tumors. It is most common in females 30-50 years of age, but it is also described in children. One study reports 1% of cases affecting children under 10 years of age and 5.9% of cases occurring in patients between the ages of 10 and 20. PA presents as a small, painless, slowly enlarging nodule. If left untreated, it can enlarge significantly, sometimes increasing by several pounds in weight. It occurs in the oral cavity, especially the palate and lips. On the palate, it is usually located in the posterior hard palate or anterior soft palate but can also be in the posterior soft palate; PA usually occurs in the posterior and lateral palate, as opposed to torus palatines, which usually occurs in the middle hard palate and in the anterior. The posterior hard palate mixed tumor is fixed due to the bone-bound anatomy of the region; the tumor is otherwise movable. Histologically, mixed tumor has a wide variety of cellular and pattern manifestations. The main cellular components are epithelial duct-like structures and mesenchymal-like tissue such as myxochondroid matrix. These lesions are generally encapsulated, ranging from predominantly myxoid (36%) to extremely cellular (12%). Complete surgical removal with clean margins is the preferred treatment. Palatal lesions respond well to excision in one piece with the periosteum and overlying mucosa. Pleomorphic adenoma has a good prognosis, but it has a tendency for recurrence (up to 44%) if not treated thoroughly. The risk of recurrence is less if it occurs in the minor salivary glands (up to 20%). The risk of malignant transformation is about 5%.
Sorry! you are incorrect
Soft-tissue neoplasms can be longstanding and asymptomatic. The clinical description of the swelling as mobile is typical of a schwannoma but the location is not typical of this condition. The age of this patient is on the older side of the typical range. Schwannomas do not have a gender predilection. The gross morphology of a yellow-tan nodule is also consistent with a neoplasm of nerve origin and the encapsulation is typical of a schwannoma. The histology, however, is not supportive of schwannoma.
Schwannoma is a benign, firm, smooth-surfaced, encapsulated and mobile neoplasm of Schwann cell origin. It occurs at any age but is more common in individuals 30-50 years of age with equal sex distribution. The tongue is the most common location, followed by the floor of mouth and the lips. It is also described as occurring within the jaw bones, especially the mandible. Up to 48% of schwannomas occur in the head-and-neck area. They are usually isolated lesions unless they present as part of neurofibromatosis type 1. Schwannoma presents as a slow-growing, firm, rubbery, smooth-surfaced nodule. The histology is usually diagnostic where the lesion is encapsulated and has two patterns: Antoni A, the cross section of which gives rise to “Verocay bodies,” and Antoni B, which is loose and resembles neurofibroma. Simple excision is the treatment of choice and recurrence is rare.