Large multilocular, expansile radiolucency left posterior mandible
Can you make the correct diagnosis?
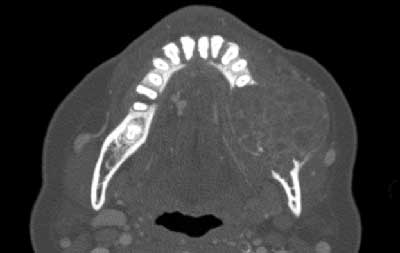
This is a 54-year-old female who presented with a chief complaint of an enlarging left mandible.
Sorry, you are incorrect!
The site being posterior mandible, the ballooning expansion of the buccal and lingual cortical bones, the multilocular radiolucency, the age of the patient and the bone loss are all strongly consistent with the clinical presentation of solid ameloblastoma. Pain is not typical of ameloblastoma’s clinical presentation and is more likely interpreted to be due to the tooth mobility and perhaps infection. The histology is not that of solid ameloblastoma. Solid ameloblastoma is one of the most common benign neoplasms of odontogenic origin. It is benign but locally aggressive; it is slow-growing and persistent. It affects a wide range of age distribution but is mostly a disease of adults, mean of 33 and an age range of 30-70 years with equal sex distribution. About 85% of ameloblastomas occur in the posterior mandible; most of these occur in the molar-ramus area. Solid ameloblastomas in general are characteristically expansile, radiolucent & multilocular in nature. They can move teeth apart and perforate and balloon the jaw bones.
Sorry, you are incorrect!
The age, gender, site, radiographic findings of multilocular and expansile radiolucency are all consistent with the clinical presentation of primary hyperparathyroidism. Hyperparathyroidism is the result of excessive production of parathyroid hormone (PTH) which is needed for calcium release. When too much PTH is present, there will be generalized bone resorption but more so in the small bones such as the jaws and the small finger bones. Primary hyperparathyroidism is usually associated with parathyroid adenoma, but possibly parathyroid hyperplasia and rarely adenocarcinoma. Primary hyperparathyroidism is 3 times more common in women and is more common in middle age females. It may produce multiple bone lesions histologically indistinguishable from central giant cell granuloma (CGCG) and that presentation is referred to as ‘brown tumor’ because of the chocolate/deep brown color of the soft tissue within the bone. This condition leads to generalized loss of density of bone with loss of lamina dura and irregular and multilocular radiolucent lesions that may be multiple and involve more than one bone. The blood workup was not consistent with the brown tumor of hyperparathyroidism and neither were the many sinusoids identified histologically.
Sorry, you are incorrect!
The multilocular and expansile radiolucency, the posterior mandible and the gender are consistent with CGCG but not the age and the involvement of the molar teeth. This lesion was more posterior than CGCG usually presents which is anterior to the first molar tooth. The histology is that of a giant cell lesion but the sinusoids are not consistent with CGCG. Central giant cell granuloma is a non-neoplastic process that can occasionally behave in a very aggressive and expansile manner, destroying bone and displacing teeth. Over 60% of CGCG cases occur in patients younger than 30 years of age, with twice as many occurrences in females as in males. Over 70% of cases occur in the mandible anterior to the first molar tooth.
Congratulations, you are correct!
The ballooning expansion of the mandible, the multilocular radiolucency, the posterior mandible, the clinical complaint of pain and the gender are all the clinical characteristics of ABC. The age of this patient however is old for ABC. Aneurysmal bone cyst is a disease of the young, usually occurs before the age 20. There is a slight predilection for females and is more common in the posterior mandible. Clinical Features include pain and swelling. Radiographically, ABC presents as multilocular or honeycombed expansile radiolucency with thinning leading to ballooning or ‘blow out’ distention of bone which is highly suggestive of ABC. The histology was that of ABC associated with a benign fibro-osseous lesion interpreted as a reactive healing process.