Generalized and persistent oral surface ulcerations
Contributed by Dr. Edward Truelove
Oral Medicine, UW-SOD, Seattle, WA
Case Summary and Diagnostic Information
This is a 44-year-old black female who presented with generalized oral ulcers since September 2016.
This is a 44-year-old black female who presented with generalized oral ulcers since September 2016 (Figure 1). Her complaint started in February 2016 with persistent sore throat, intermittently, for several months that did not respond to antibiotics or antiviral treatment. In September she developed multiple/generalized painful oral ulcers that made it difficult for her to eat and thus lost 34lb. At that time, she also noted abdominal and thigh ulcers and developed pain and redness in her eyes. The eye lesions responded to prednisone eye drops.

Figure 1 This is a clinical photograph taken of the patient when she was admitted to the University of Washington Medical Center. Note the severe ulceration and swelling of both lips, especially the lower lip. Also, note the ulceration of the soft palate area.
The patient’s past medical history is significant for sickle cell trait but otherwise is healthy. She denies medication allergies. No history of immune compromised conditions.
Patient developed sore throat in February 2016 which persisted and was intermittent for several months without evidence of obvious lesions. In May 2016 she was treated with antibiotics but symptoms persisted. In July, she was treated with magic mouthwash and omeprazole and a small ulcerated lesion was noted on the left posterior tonsil. Culture was done and was negative except for normal respiratory flora. She did not respond to Acyclovir either. By September she developed multiple oral ulcers involving both upper and lower lips, tongue and soft palate (Figures 1-2). Oral ulcers were painful making it hard for her to eat and lost 34lb. She also noted ulcers on her abdomen, thigh and vulva which were also painful. There was concern for potential ocular involvement as she developed pain and redness in her eyes without blurred vision and was seen by an ophthalmologist; she responded to prednisone eye drops. Ulcers were also found on the oropharynx, and vagina.

Figure 1 This is a clinical photograph taken of the patient when she was admitted to the University of Washington Medical Center. Note the severe ulceration and swelling of both lips, especially the lower lip. Also, note the ulceration of the soft palate area.

Figure 2 Closer look at the swollen and ulcerated upper and lower lips.
Over the six months period this patient was treated with several courses of antibiotics and antiviral drugs without much response.
Histologic examination reveals a hemisected piece of soft tissue composed of surface epithelium splitting above the basal cell layer (Figure 3-4). The spinous layer shows evidence of acantholysis and the basal cell layer is intact and part of the detached connective tissue. The latter is infiltrated by a mixed inflammatory population. Direct immunofluorescent staining shows positive intercellular staining of the spinous layer cells with antibody to IgG and C3 (Figures 5-6).
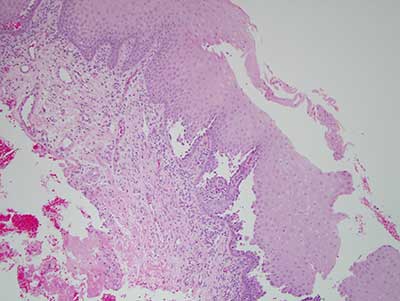
Figure 3 This is a low power (100X) photograph of an H & E stained section, demonstrating a split of the surface epithelium above the basal cell layer. The latter is intact and part of the detached connective tissue. There is evidence of breakdown of the spinous layer epithelial cells (acantholysis). The connective tissue is infiltrated by mixed and chronic inflammatory cells.
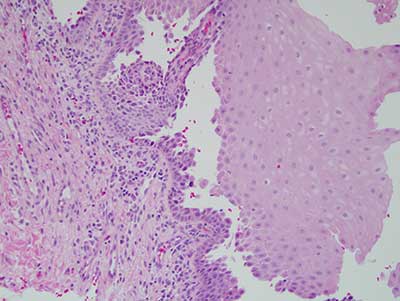
Figure 4 This is a higher power (200X) photograph of an H & E stained section, focusing on the split of the surface epithelium and the breakdown of the spinous layer epithelial cells (acantholysis).
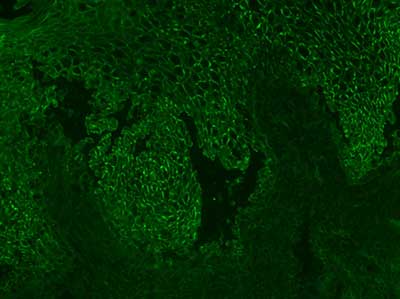
Figure 5 This is a higher power (200X) photograph of a direct immunofluorescence stain demonstrating positive staining with antibody to IgG. Note the “apple-green” fine line positive intercellular stain around the spinous layer cells.
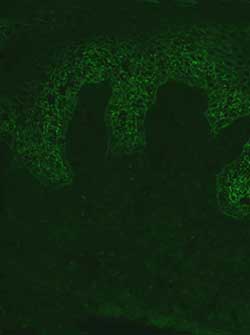
Figure 6 This is a higher power (200X) photograph of a direct immunofluorescence stain demonstrating positive staining with antibody to C3. Note the “apple-green” fine line positive intercellular stain around the spinous layer cells.
After you have finished reviewing the available diagnostic information