Large & Well-Demarcated Radiolucency Left Posterior Mandible
Can you make the correct diagnosis?
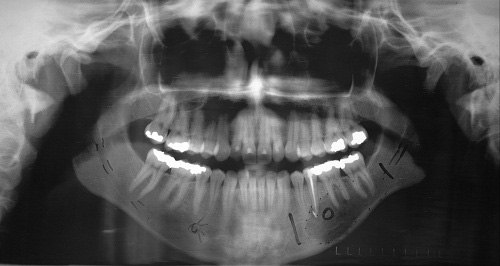
This is a 21-year-old white female with a four-month history of radiolucency in the left posterior mandible.
Sorry! you are incorrect
A unilocular radiolucency associated with an endodontically treated tooth should make one think of a periapical cyst. Another cyst to consider would be an odontogenic keratocyst. Lack of expansion would be more consistent with OKC but periapical cyst would be certainly considered given the endodontically treated tooth present in the area. Pain is described in both cysts if they are infected.
Given the radiographic findings of a unilocular and well-defined radiolucency one has to consider a cyst(s) on the differential diagnosis. Being closely associated with the apex of an endodontically treated tooth #20, a radicular cyst would be a reasonable consideration. The histology is not supportive of a periapical cyst.
Apical periodontal cyst is also known by a variety of other names, including radicular and periapical cyst. It is an inflammatory cyst and is the most common odontogenic cyst. It is the result of pulpitis/pulp necrosis, which are mainly caused by a badly decayed tooth but can also be the result of tooth fracture, failed endodontic treatment or an old filling with secondary caries. It can occur at any age but is more common in adults in their fourth and fifth decade of life. It is usually present at the apex of a tooth but can be apical lateral to a tooth. It is usually asymptomatic and small (around 0.5-1.5 cm) in size but can occasionally reach large sizes. It can be symptomatic, i.e. painful and expansile, if infected. The infected cysts may break through the cortical bone in the form of a fistula, usually buccal or labial in the mandible and buccal or palatal in the maxilla. It is more common in males than females and slightly more common in the maxilla, especially the anterior maxilla. Radiographically, it presents as a well-demarcated or corticated unilocular radiolucency at the apex of a tooth or apical and lateral of a tooth. Occasionally, the radicular cyst can be multilocular. It can also be associated with root resorption, but rarely. Histologically, it is made up of a cystic structure lined by epithelium and supported by a connective tissue wall. The latter is usually chronically inflamed and frequently associated with abscess. Treatment ranges from conventional endodontic treatment to apicoectomy to extraction of the tooth with curettage of the cystic structure. It has a good prognosis.
Sorry! you are incorrect
A unilocular radiolucency associated with an endodontically treated tooth should make one think of a periapical cyst. Another cyst to consider would be an odontogenic keratocyst. Lack of expansion would be more consistent with OKC but periapical cyst would be certainly considered given the endodontically treated tooth present in the area. Pain is described in both cysts if they are infected.
Given the radiographic findings of a unilocular and well-defined radiolucency, a cyst has to be on the differential diagnosis. OKC is considered high up on the differential diagnosis given the lack of expansion but the histology is not supportive of OKC.
The odontogenic keratocyst (OKC) is an aggressive odontogenic cyst, known for its rapid growth and its tendency to invade the adjacent tissues, including bone. It has a high recurrence rate and is associated with basal cell nevus syndrome. It affects patients in the age ranges of 20-29 and 40-59, but cases in patients ranging in age from 5 to 80 years have been reported. The distribution between sexes varies from equal distribution to a male-to-female ratio of 1.6:1, except in children. Odontogenic keratocysts may occur in any part of the upper and lower jaw, with the majority (almost 70%) occurring in the mandible. They occur most commonly in the angle of the mandible and ramus. Anterior maxilla is a rare location for OKC but has been described. Radiographically, OKCs present predominantly as unilocular radiolucencies with well-defined or sclerotic borders; they may also present as multilocular radiolucencies, but rarely. OKCs commonly present as a unilocular radiolucency with scalloped borders. Teeth associated with OKC are vital. OKCs grow to sizes larger than any other odontogenic cysts. They usually penetrate the bone rather than expand it and grow in an anterior to posterior direction. Despite this aggressive growth, they often remain asymptomatic, thus growing to large sizes and hollowing the bone. Treatment of choice is surgery with cauterization, especially with Carnoy’s solution.
Congratulations! You are correct
Alveolar soft part sarcoma (ASPS) is a rare malignant neoplasm that is of unknown cell differentiation. Skeletal muscle differentiation has been proposed but is not strongly supported. ASPS is a slow-growing malignancy with a high propensity for metastasis; therefore early detection and treatment is important.
Clinically, it is more common in adolescent or young adults, with predilection for occurrence in young females. In at least two studies, females were found to be predominant (68-71%) among patients less than 30 years of age and males were predominant (67-68%) among patients over 30 years of age. It is more commonly described in the lower limb and around the limb girdle. These tumors are slow growing but have a very high predilection for metastasis, especially to the lungs, brain, bone, liver, spleen and other unexpected areas such as the female genital tract cervix and uterus. There is only one published report (from 2010) that describes metastasis to the mandible. This patient was known to have ASPS which metastasized to the mandible after one year of diagnosis. Most series have suggested that ASPS is resistant to conventional chemotherapy agents and that complete surgical excision is the treatment of choice for primary and metastatic lesions. Radiotherapy as a treatment for ASPS is still not well studied, but anti-angiogenic types of medications show a promising outcome. Survival seems to be associated with age and the size of the tumor at diagnosis; older patients and tumors larger than 10 cm have a poor prognosis. Larger tumor size appears to be associated with increased risk of distant metastases in adult patients. One study showed the median survival of 26 patients was 90 months, with overall 5- and 10-year survival rates of 64% and 48%, respectively, but the median survival for those with stage IV disease at initial diagnosis was 41 months. ASPS has a 30% incidence of brain metastases. These have a much poorer prognosis; patients typically survive one year after diagnosis.
References
- Souza LB, Gordón-Núñez MA, Nonaka CF, Medeiros MC, Torres TF, Emiliano GB. Odontogenic cysts: demographic profile in a Brazilian population over a 38-year period. Med Oral Patol Oral Cir Bucal. 2009 Dec 29.
- Avelar RL, Antunes AA, Carvalho RW, Bezerra PG, Oliveira Neto PJ, Andrade ES. Odontogenic cysts: a clinicopathological study of 507 cases. J Oral Sci. 2009 Dec;51(4):581-6.
- Damm DD, Fantasia JE. Oral diagnosis. Radiolucency of anterior maxilla. Odontogenic keratocyst. Gen Dent. 2005 Jul-Aug;53(4):308, 310.
- Shear M. Odontogenic keratocysts: natural history and immunohistochemistry. Oral Maxillofacial Surg Clin N Am. 2003; 15: 347-362.
- Oda D, Rivera V et al. Odontogenic keratocyst: the northwestern USA experience. J Contemp Dent Pract. 2000 Feb 15; 1(2): 60-74.
- Reichart PA, Philipsen HP. et al. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol 1995;31B:86–99.
- Julio César Bisinelli, Sérgio Ioshii, Luciana Borges Retamoso, Simone Tetü Moysés, Samuel Jorge Moysés and Orlando Motohiro Tanaka. Conservative treatment of unicystic ameloblastoma. American Journal of Orthodontics and Dentofacial Orthopedics. Volume 137, Issue 3, March 2010, Pages 396-400.
- Rocha LA, Rizo VH, Romañach MJ, de Almeida OP, Vargas PA. Oral metastasis of alveolar soft-part sarcoma: a case report and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010 Apr;109(4):587-93.
Sorry! you are incorrect
The age of the patient, the location and the unilocular radiolucency are all supportive of this diagnosis and therefore should stay on the differential diagnosis. The lack of expansion and the lack of association with an impacted tooth argue against the diagnosis of a unicystic ameloblastoma since 90% of these cases present looking like a dentigerous cyst.
Ameloblastoma is one of the most common benign neoplasms of odontogenic origin. It accounts for 11% of all odontogenic neoplasms. It is a slow-growing, persistent, and locally aggressive neoplasm of epithelial origin. It affects a wide range of age distribution but is mostly a disease of adults, at an average age of 33, with equal sex distribution. The unilocular radiolucency is more consistent with unicystic ameloblastoma. 90% of unicystic ameloblastomas are associated with the crown of an impacted tooth. The other 10% are unilocular radiolucency usually associated with teeth such as between teeth. The patients constituting this group are around 14-20 years of age. Curettage is the treatment of choice for luminal and plexiform types of unicystic ameloblastomas and en-bloc or resection are an option for the mural type. The recurrence rate ranges from 6-35% depending on the type.