Dome shaped, smooth-surfaced swelling, floor of mouth
Can you make the correct diagnosis?
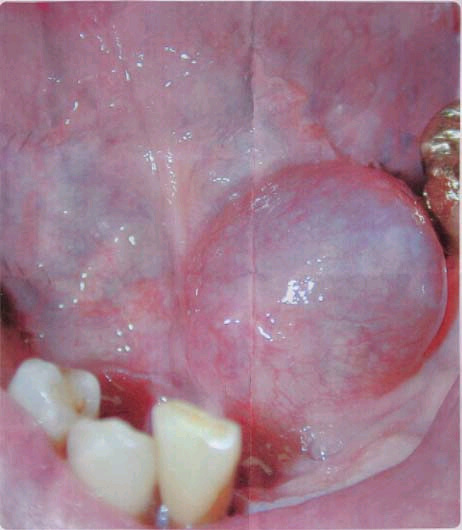
This is a 67-year-old male with a smooth-surfaced, dome-shaped and pink- to grayish-blue swelling located off the midline in the left side of the floor of mouth.
Sorry! you are incorrect
This is a malignant neoplasm of salivary gland origin that can present as a smooth-surfaced swelling or a non-healing ulcer on the palate. Three histologic types are reported: low, intermediate and high; the low-grade type is more common in the oral cavity (1). Mucoepidermoid carcinoma accounts for 10% of all salivary gland neoplasms (1-2). While the majority of cases occur in the parotid gland, some also occur in minor salivary glands, especially the palate, tongue, buccal mucosa, lips, and retromolar pad areas (1-4). It can occur at any age, but with a predilection for young people (1-2). Armed Forces Institute of Pathology (AFIP) studies demonstrate that 44% of cases occur in patients under 20 years of age, most commonly on the palate (1); their youngest patient was nine months old. The low-grade lesions are slow-growing and painless, and not encapsulated; they sometimes resemble a mucocele, especially those at the retromolar pad area (1-2). Retromolar pad area mucoceles are rare, and for that reason it is best to biopsy early to exclude the possibility of a mucoepidermoid carcinoma masquerading as a mucocele. High-grade lesions tend to be more common in the parotid gland. These present as rapidly growing, painful lesions with facial nerve paralysis and sometimes with regional lymph node metastasis. Histologically, mucoepidermoid carcinoma consists of a variety of cell types and architectural patterns which constitute the three histologic gradings. Although low-grade mucoepidermoid carcinoma is characterized by an abundance of mucous-producing cells and duct-like structures with cystic dilation, the mere presence of certain types of cells and architecture should not be used to determine the histologic grade. Complete surgical removal with clean margins is the preferred treatment for the low-grade type. Radiotherapy has also been successfully used, especially when the tumor involves the surgical margins (1-5). Neither the site nor the histology in this case is supportive of a mucoepidermoid carcinoma.
Sorry! you are incorrect
This cyst usually occurs in the ovaries of young females (6-7), and is rare in the oral cavity. It is a teratoma in that all three germ cell layers are found in the cystic structure (6-7). The form of this cyst as it occurs in the oral cavity is simpler than its more common ovarian counterpart. Most oral dermoid cysts contain the skin adnexa in their connective tissue wall, including hair, but not much of other tissues (8). Oral dermoid cyst presents as a large, round, raised, smooth-surfaced, dome-shaped nodule in the floor of mouth, usually in the middle of the floor of mouth pushing the tongue upward (6-8). It is typically the same color as the surrounding tissue, whereas this case was slightly blue in color (6-8). It is painless but can interfere with eating, speaking and swallowing if large in size (6-8). The histology consists of a cystic cavity lined by epithelium and supported by a connective tissue wall. The latter contains skin adnexa, including hair follicles (8). Other tissue, including brain, has been identified within the wall. Conservative surgical excision is the treatment of choice. It has a good prognosis. The clinical presentation in this case is suggestive of a dermoid cyst, but the color, age and sex of the patient and the histology are not supportive of this disease.
Sorry! you are incorrect
Lipomas are benign neoplasms of adipose tissue origin which are extremely common in the subcutaneous tissue of the extremities and trunk, but not in the oral cavity, hands and feet. This neoplasm rarely occurs in children and is more common in adults over the age of 30 with equal gender distribution (9-11). It is usually single, but can present in multiples, and is slow- growing and painless. Floor of mouth, tongue and buccal mucosa are the most common locations of occurrence in the oral cavity (10-11). Depending on the size of the lesion, it can be smooth surfaced or lobulated. It is usually yellowish in color and sessile, with a thin surface and visible blood vessels. Lipomatous nodules of the buccal mucosa may represent herniation of the buccal fat pad (10-11). Because of its softness, it can be mistaken for a cyst. Histologically, this neoplasm is usually made up of lobules of mature adipocytes surrounded by fibrous connective tissue (9-11). Simple surgical excision is the treatment of choice, and recurrence is rare. In this case, the swelling in the floor of mouth is suggestive of a lipoma. However, neither the color nor the histology supports this diagnosis.
Congratulations! You are correct
Mucoceles and ranulas are clinical terms describing exophytic, fluid-filled, fluctuant nodules, typically of minor salivary gland origin, which present mostly on the lower lip (mucocele) and the floor of mouth (ranula) (12-14). Over 90% of these lesions are cyst-like structures, or pseudocysts, and are mucous extravasation phenomena referred to as mucoceles. Some of these lesions are true cystic structures lined by epithelium and filled with mucus. These are called mucus retention cysts or salivary duct cysts; they constitute a small percentage of all mucoceles (12-14). Ranulas, mucoceles of the floor of the mouth, constitute less than 10% of all mucoceles and are divided into those located above the mylohyoid muscle (the majority, like our case) and below the mylohyoid muscle (also known as plunging ranulas or cervical ranulas) (12-15). Ranulas are of minor or major salivary gland origin and are mostly extravasation in type. The etiology of the extravasation mucoceles is usually sharp trauma cutting through the salivary gland duct and releasing the mucous in the extracellular tissue (12-14). Histologically, the extravasation-type mucocele consists of a cyst-like structure lined by granulation tissue and filled with mucoid material, foamy macrophages, and at times small clusters of neutrophils. The mucous retention cysts develop as a result of a duct blockage which can be caused by trauma, fibrosis, sialolith, or pressure from an overlying tumor (13-14). The extravasation mucoceles most commonly occur on the lower lip and are extremely rare on the upper lip. They may occur anywhere else in the oral cavity, including the buccal mucosa and floor of mouth (i.e. ranula). The latter can be of minor salivary gland or submandibular or sublingual gland duct origin (14-15). It is more commonly seen in children and adolescents. It presents as a swelling with a bluish color if superficial, while deep mucoceles tend to take the color of the surrounding mucosa. Mucoceles tend to fluctuate in size. They are usually associated with a history of sharp lip or cheek biting, but can also be secondary to surgery in the area. This is especially true with the anterior tongue mucoceles. Surgical excision with the associated minor salivary gland is the preferred treatment for deep mucoceles; superficial mucoceles can self-heal within 2-3 weeks. Superficial mucoceles can also mimic vesiculobullous-type diseases because they look like vesicles (13), especially when presenting in multiples (rare, but described). They can recur if the source of trauma is not eliminated or if they are secondary to surgery. Simple (non-plunging) ranula is best treated by marsupialization into the floor of mouth (15). Plunging ranula requires complete excision via an extra-oral approach. The technical difficulties associated with the complete removal of this thin-walled lesion result in a relatively high recurrence rate. There is no evidence of recurrence as of this date.
Treatment
Under local anesthesia, the lesion was completely removed and submitted for microscopic examination. Some of the surrounding minor salivary glands were also surgically removed. The healing was complete with no complications.
References
- Auclair PL, Ellis GL. Mucoepidermoid carcinoma. In Ellis GL, Auclair PL, Gnepp DR, editors. Surgical pathology of the salivary glands. Philadelphia: W.B. Saunders, 1991. p. 269-298.
- Hicks J, Flaitz C. Mucoepidermoid carcinoma of salivary glands in children and adolescents: assessment of proliferation markers. Oral Oncol. 2000 Sep;36(5):454-60
- Bentz BG, Hughes CA, Ludemann JP, Maddalozzo J. Masses of the salivary gland region in children. Arch Otolaryngol Head Neck Surg. 2000 Dec;126(12):1435-9.
- Epstein JB, Hollender L, Pruzan SR. Mucoepidermoid carcinoma in a young adult: recognition, diagnosis, and treatment and responsibility. Gen Dent. 2004 Sep-Oct;52(5):434-9.
- Chigurupati R, Alfatooni A, Myall RW, Hawkins D, Oda D. Orofacial rhabdomyosarcoma in neonates and young children: a review of literature and management of four cases. Oral Oncol. 2002 Jul;38(5):508-15.
- Seah TE, Sufyan W, Singh B. Case report of a dermoid cyst at the floor of the mouth. Ann Acad Med Singapore. 2004 Jul;33(4 Suppl):77-9.
- Longo F, Maremonti P, Mangone GM, De Maria G, Califano L. Midline (dermoid) cysts of the floor of the mouth: report of 16 cases and review of surgical techniques. Plast Reconstr Surg. 2003 Nov;112(6):1560-5.
- Santos-Briz A Jr, Serrano R, del Canizo A, Santos-Briz A, de Agustin PP. Liesegang rings in a dermoid cyst of the floor of the mouth. Report of a case with cytologic findings. Acta Cytol. 2000 Nov-Dec;44(6):1062-5.
- Clark S, Greenwood M, Fullarton M, Russell JS. An unusual case of floor of mouth swelling: case report, differential diagnosis and a review of the literature. Dent Update. 2005 Dec;32(10):617-9.
- Furlong MA, Fanburg-Smith JC, Childers EL. Lipoma of the oral and maxillofacial region: Site and subclassification of 125 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004 Oct;98(4):441-50.
- Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA. Lipomas of the oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg. 2003 Feb;32(1):49-53.
- Kopp WK, St-Hilaire H. Mucosal preservation in the treatment of mucocele with CO2 laser. J Oral Maxillofac Surg. 2004 Dec;62(12):1559-61.
- Silva A Jr, Nikitakis NG, Balciunas BA, Meiller TF. Superficial mucocele of the labial mucosa: a case report and review of the literature. Gen Dent. 2004 Sep-Oct;52(5):424-7. Review
- Taglialatela Scafati C. Mucoceles as a complication of submandibular intubation. J Craniomaxillofac Surg. 2004 Oct;32(5):335.
- Yuca K, Bayram I, Cankaya H, Caksen H, Kiroglu AF, Kiris M. Pediatric intraoral ranulas: an analysis of nine cases. Tohoku J Exp Med. 2005 Feb;205(2):151-5
- Waldrom CA. Mixed tumor (pleomorphic adenoma) and myoepithelioma. In Ellis GL, Auclair PL, Gnepp DR, editors. Surgical pathology of the salivary glands. Philadelphia: W.B. Saunders, 1991. p. 165-186.
- Hockstein NG, Samadi DS, Gendron K, Carpentieri D, Wetmore RF. Pediatric submandibular triangle masses: a fifteen-year experience. Head Neck. 2004 Aug;26(8):675-80.
- Foote FW Jr., Frazell EL. Tumors of the major salivary glands. Atlas of tumor pathology, Section IV, Fascicle 11, 1st Series. Washington DC: Armed Forces Institute of Pathology, 1954.
- da Cruz Perez DE, Pires FR, Alves FA, Almeida OP, Kowalski LP. Salivary gland tumors in children and adolescents: a clinicopathologic and immunohistochemical study of fifty-three cases. Int J Pediatr Otorhinolaryngol. 2004 Jul;68(7):895-902.
Sorry! you are incorrect
The floor of mouth is a very unusual location for mixed tumor. It is the most common benign salivary gland neoplasm of both the major and minor salivary glands. It originates from the myoepithelial cells and the reserve cells of the intercalated ducts. It accounts for 80% of all benign salivary gland neoplasms. It occurs in both major and minor salivary glands and accounts for up to 77% of parotid, 68% of submandibular, and 43% of minor salivary gland tumors (16). It is more common in females 30-50 years of age, but it is also described in children (16, 19). It presents as a small, painless, slowly enlarging nodule. If left untreated it can enlarge significantly, sometimes growing to several pounds in weight (16-18). It occurs in the oral cavity, especially the palate and lips (19). The palatal mixed tumor is fixed due to the bone-bound anatomy of the region. The tumor is otherwise movable. Histologically, mixed tumor has a wide variety of cellular and pattern manifestations; the main cellular components are epithelial duct-like structures and mesenchymal-like tissue such as myxochondroid matrix. These lesions are generally encapsulated, ranging from predominantly myxoid (36%) to extremely cellular (12%) (16-17). Complete surgical removal with clean margins is the preferred treatment (16-19). Palatal lesions respond well to excision in one piece with the periosteum and overlying mucosa. The prognosis is good, but it has a tendency for recurrence (up to 44%) if not treated thoroughly (16). The risk of recurrence is lower in the minor salivary glands (up to 20%). The risk of malignant transformation is about 5% (16). The site in this case is not supportive of mixed tumor; nor is the histology.