Very large Scalloped & Multilocular Radiolucency Associated with Impacted Tooth #32
Can you make the correct diagnosis?
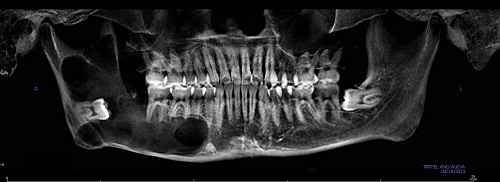
This is a 23-year-old Asian male referred by his general dentist for a deeply impacted tooth # 32 associated with a very large, scalloped and multilocular radiolucency starting from tooth #28 and extending superiorly into the high ramus.
Sorry! you are incorrect
The radiographic presentation of a radiolucency associated with the crown of an impacted tooth is by definition a dentigerous cyst (DC). The impacted tooth is mandibular third molar tooth, which also supports the clinical presentation of a dentigerous cyst. The age of the patient is also consistent with the condition. However, the size of the radiolucency and, especially, the lack of expansion are not consistent with a dentigerous cyst; neither is the perforation of bone. The multilocular radiolucency can be consistent with a DC, but this is uncommon. The histology is not supportive of a diagnosis of DC.
Dentigerous cyst is the most common developmental cyst in the oral cavity, accounting for 20% of the developmental cysts of the jaws, and is almost always associated with the crown of a tooth attached to the cemento-enamel junction, as is the case in this patient. It is believed to originate from the accumulation of fluid between the reduced enamel epithelium and the tooth crown, thus expanding the follicle beyond the 3 mm normal diameter. It is usually associated with impacted or un-erupted teeth. Clinically, it can be an asymptomatic radiolucency discovered during a routine dental examination or can act aggressively by expanding the jaws, leading to facial asymmetry with extreme displacement of adjacent teeth as well as the involved tooth. It can be painful and cause root resorption, especially if it is infected. It is more common in the third molars and upper canines and can also involve supernumerary teeth and odontomas. Radiographically, it presents as a smooth border, usually unilocular or sometimes multilocular radiolucency, located around the tooth circumferentially, laterally or in the form of a “doughnut” ring. The size varies from small to extremely large, extending into the ramus of the mandible. The borders are usually corticated and smooth unless it is inflamed when loss or cortication (usually partial) is present. Histologically, the cyst has non-specific features lined by variable thickness of stratified squamous epithelium and supported by connective tissue. Clusters of mucous cells are frequently present, especially in the mandibular third molar areas. Treatment depends on its size, and ranges from thorough curettage to marsupialization. It usually has a good prognosis. Recurrence is uncommon if it is properly removed. Occasionally this cyst is associated with ameloblastoma, epithelial dysplasia and/or squamous cell carcinoma or mucoepidermoid carcinoma.
Congratulations! You are correct
The age, the site and the clinical presentation of being asymptomatic, lacking expansion and yet hollowing through the bone from the body of the mandible to the superior ramus are all typical of odontogenic keratocyst (OKC). The perforation of bone also supports this diagnosis, as does the radiographic finding of a scalloped radiolucency. However, the radiolucency is also multilocular; this does not argue against OKC as a possible diagnosis, but it is less common than the presentation of a unilocular radiolucency with a scalloped border. The histology is consistent with OKC.
Odontogenic keratocyst (OKC) is an aggressive odontogenic cyst and is known for its rapid growth and its tendency to invade the adjacent tissues, including bone. It has a high recurrence rate and is associated with basal cell nevus syndrome. The majority of patients are in the age ranges of 20-29 and 40-59, but cases in patients ranging in age from 5 to 80 years have been reported. The distribution between sexes varies from equal distribution to a male-to-female ratio of 1.6:1. OKC predominantly affects Caucasian populations and, if one may judge from the limited evidence provided by the literature, is chiefly of Northern European descent. Odontogenic keratocysts may occur in any part of the upper and lower jaw, with the majority (almost 70%) occurring in the mandible. They occur most commonly in the angle of the mandible extending superiorly into the ramus. Radiographically, OKCs present predominantly as unilocular radiolucencies with well-defined or sclerotic borders; they may also present as multilocular radiolucencies or unilocular radiolucencies with scalloped borders (the latter is more common). They usually penetrate the bone rather than expand; they grow in an anterior and posterior manner with little to no expansion. Larger OKCs, however, tend to expand bone, but mildly. Obvious clinical expansion should be viewed with suspicion for a neoplasm. OKCs can also present as small and oval radiolucencies between teeth simulating a lateral periodontal cyst, in an area of an extracted tooth simulating a residual cyst, at the apex of a vital tooth mistaken for a periapical cyst, or in the anterior maxilla between the central incisors simulating an incisive canal cyst. OKCs grow to sizes larger than any other odontogenic cysts. Despite this aggressive growth, they often remain asymptomatic, thus growing to large sizes and hollowing the bone. Like dentigerous cysts, if infected, they can be painful, thus symptomatic. Multiple OKCs are frequently associated with bifid-rib basal cell nevus syndrome (Gorlin syndrome). Odontogenic keratocysts are significant clinical entities due to their tendency for recurrence and destructive behavior. They are known to have a high recurrence rate, ranging from 13% to 60%. Complete surgical removal is the treatment of choice. Enucleation combined with Carnoy’s solution or liquid nitrogen treatment has been effective in reducing the recurrence rate.
References
- Hyomoto M, Kawakami M, Inoue M, Kirita T. Clinical conditions for eruption of maxillary canines and mandibular premolars associated with dentigerous cysts. Am J Orthod Dentofacial Orthop. 2003; 124:515-520.
- Shibata Y, Asaumi J, Yanagi Y, Kawai N, Hisatomi M, Matsuzaki H, Konouchi H, Nagatsuka H, Kishi K. Radiographic examination of dentigerous cysts in the transitional dentition. Dentomaxillofac Radiol. 2004 Jan;33(1):17-20.
- Ko KS, Dover DG, Jordan RC. Bilateral dentigerous cysts–report of an unusual case and review of the literature. J Can Dent Assoc. 1999 Jan;65(1):49-51.
- Shear M. Odontogenic keratocysts: natural history and immunohistochemistry. Oral Maxillofacial Surg Clin N Am. 2003; 15: 347-362.
- Oda D, Rivera V et al. Odontogenic keratocyst: the northwestern USA experience. J Contemp Dent Pract. 2000 Feb 15; 1(2): 60-74.
- Zachariades N, Papanicolaou S, Triantafyllou D. Odontogenic keratocysts: Review of the literature and report of sixteen cases. J Oral Maxillofac Surg. 1985; 43: 177-182.
- Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol 1995;31B:86–99.
- Adekeye EO, McLavery K. Recurrent ameloblastoma of the maxillofacial region. Clinical features and treatment. J Maxillofac Surg 1986;14:153-157.
- Gardner DG. Some current concepts on the pathology of ameloblastomas. J Oral Maxillofac Surg 1996;82:660-669.
Sorry! you are incorrect
The site, the multilocular radiolucency and the bone perforation are consistent with ameloblastoma. However, the obvious lack of expansion argues against ameloblastoma. As to the age, the young age and the association with an impacted tooth is consistent with a unicystic ameloblastoma but is not consistent with the conventional (multicystic) ameloblastoma which the multilocular radiolucency is implying. The histology is not consistent with ameloblastoma, unicystic or otherwise.
Ameloblastoma is defined as a benign neoplasm of tooth origin and as a benign but locally aggressive neoplasm with potential for invasion of the surrounding bone and soft tissue. It also has the potential for local extension to the brain, resulting in the death of the patient. However, not all ameloblastomas behave in an aggressive manner; ameloblastoma is a family of diseases with different biological behaviors. Therefore, it is necessary to distinguish between the various types before a definitive treatment is rendered. Four clinical types are described, beginning with the solid type (radiographically multilocular) which is treated with complete resection or en bloc (partial) resection depending on the size. The unicystic type includes three histologic types, one of which (mural cystic ameloblastoma) behaves like the solid type, while the other two types (intraluminal and plexiform unicystic) are less aggressive and treated with curettage. The other two types of ameloblastoma are peripheral (extra-osseous), treated with conservative surgical removal, and desmoplastic ameloblastoma, which is treated with en bloc or resection similar to the solid form.
The multilocular radiographic presentation in this case would support a diagnosis of solid ameloblastoma but not the age of the patient. Solid ameloblastoma is a slow-growing, persistent, and locally aggressive neoplasm of odontogenic epithelial origin. It affects a wide range of age distribution but is mostly a disease of adults, at an average age of 33, with equal sex distribution. Reports from Africa and India show a male predilection; it is also particularly prevalent in patients of black origin.
About 85% of ameloblastomas occur in the posterior mandible, most in the molar-ramus area, with few occurring in the anterior mandible. About 15% occur in the maxilla, the vast majority in the posterior maxilla. Ameloblastomas of the maxilla tend to occur in an older age population. Solid ameloblastoma, if not treated, can reach very large sizes with facial disfiguring. It loosens, displaces and resorbs adjacent teeth. With the exception of jaw expansion, it is usually asymptomatic unless infected, where it can be mildly painful. Parasthesia and anesthesia are extremely rare, unless they are very large in size. If ameloblastoma perforates bone with extension into the adjacent soft tissue, it has a higher tendency for recurrence and therefore has a worse prognosis than those completely encased by bone.
The solid type is treated with complete surgical removal with clean margins through resection or en bloc. Curettage is not recommended for the solid type because it is associated with a higher recurrence rate than the resected counterpart. Resected jaws may require secondary reconstruction. It has an overall good prognosis but is known to have a high recurrence rate, particularly in the posterior maxilla, inadequate surgery (tumor extending to the surgical margins). Long-term follow-up is required. Recurrence is related to the treatment modality. Patients should be placed on follow-up for at least five years.