Return to Case of the Month Archives
Generalized Ulcerative Oral Mucosa
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Contributed by: Drs. Michael Martin and Brian Jackson
Department of Oral & Maxillofacial Surgery, UW, Seattle, WA
Case Summary and Diagnostic Information

This is a 14-year-old white male who was referred to the Department of Oral Medicine, UW SOD with a chief complaint of not being able to eat or drink because of generalized oral ulcers and sloughing epithelium.
Diagnostic Information Available
This is a 14-year-old white male who came to the Department of Oral Medicine of the University of Washington, School of Dentistry with a chief complaint of not being able to eat or drink because of generalized oral ulcers and sloughing epithelium that had been present for eight weeks. The ulcers started at the mucosal area of the lower inner lip (Figure 1) and later spread to his entire mouth except for the outer lips. This included the gingiva, bilateral buccal mucosae and vestibules (Figure 2), the floor of his mouth (Figure 3), the soft palate and throat (Figure 4), and inner lips. He was given a Benadryl and Maalox rinse as well as amoxicillin, to no effect. He was having difficulty eating and drinking and as a result lost 15 pounds. Extra-orally, he developed sores in his left eye which responded to eye drops and ointment, and later in his right eye which responded to anti-inflammatory ointment but recurred.

Figure 1. This is a clinical view of the lesions at the first week of January 2011 demonstrating generalized ulceration of the lower lip. The ulcers are superficial and irregular and are covered by pseudomembrane.

Figure 2. This is a clinical view of the lesions at the second week of January 2011 demonstrating generalized ulceration of the mandibular vestibule and buccal mucosa. Like the other areas of the mouth, the ulcers are superficial and irregular and are covered by pseudomembrane.

Figure 3. This is a clinical view of the lesions at the first week of January 2011 demonstrating generalized ulceration of the floor of mouth. Like the lower lip, the ulcers are superficial and irregular and are covered by pseudomembrane.

Figure 4. This is a clinical view of the lesions at the first week of January 2011 demonstrating generalized ulceration of the uvula and soft palate area. Like the other areas of the mouth, the ulcers are superficial and irregular and are covered by pseudomembrane.
The patient’s past medical history is significant for asthma, which he has outgrown. His family history is significant for eczema and thyroid auto-immune disease.
This patient developed ulcers on the mucosa of the inner lower lip (Figure 1) shortly after Thanksgiving, 2010. About 2 weeks later, he was first evaluated for this at his pediatrician’s office. He was given a Benadryl and Maalox rinse. The ulcers and sloughing of the epithelium continued to get worse and spread all over his mouth (Figure 2-4). He complained of throat pain and difficulty eating and drinking. The ulcers were never on the outer lips. He was seen again by his pediatrician and prescribed a course of amoxicillin, which did not have any effect. His symptoms continued to get worse, to the point where he could not eat or drink. He was seen by Dr. Jackson and later by Dr. Martin of the Department of Oral Medicine at the University of Washington. At one point, he went to Seattle Children’s Emergency Department for dehydration and was given pain medications, a mouthwash, and was rehydrated. Dr. Martin of Oral Medicine started him on oral prednisolone (15 mg/5 mL) 3 mL p.o. b.i.d., which he took for 3 weeks, as well as dexamethasone mouthwash, which he used 3 times daily. His mouth healed with just two residual ulcers that would not go away. As he continued to have multiple persistent lesions, Dr. Martin recommended stopping the prednisone for 48 hours and do a repeat biopsy, and his sores flared within those 48 hours. ?He resumed oral prednisolone (15 mg/ 5 mL) at 3 mL p.o. twice daily. The results of the second biopsy led to a referral to Children’s Hospital, Department of Dermatology for a definitive treatment. While the oral lesions were ongoing, the patient developed sores in his eyes, starting with the left eye and then the right eye.

Figure 1. This is a clinical view of the lesions at the first week of January 2011 demonstrating generalized ulceration of the lower lip. The ulcers are superficial and irregular and are covered by pseudomembrane.

Figure 2. This is a clinical view of the lesions at the second week of January 2011 demonstrating generalized ulceration of the mandibular vestibule and buccal mucosa. Like the other areas of the mouth, the ulcers are superficial and irregular and are covered by pseudomembrane.

Figure 3. This is a clinical view of the lesions at the first week of January 2011 demonstrating generalized ulceration of the floor of mouth. Like the lower lip, the ulcers are superficial and irregular and are covered by pseudomembrane.

Figure 4. This is a clinical view of the lesions at the first week of January 2011 demonstrating generalized ulceration of the uvula and soft palate area. Like the other areas of the mouth, the ulcers are superficial and irregular and are covered by pseudomembrane.
Treatment
The plan for treatment included performin and indirect IMF staining to confirm the diagnosis of pemphigus vulgaris, as well as increasing the prednisone dosage to 60 mg p.o. daily, taken as pills. He was also started on ranitidine 150 mg p.o. daily for GI prophylaxis and given calcium and vitamin D supplements. In addition, he started on CellCept, (mycophenolate mofetii) 500 mg p.o. b.i.d., for 1 week. This was then increased to 1000 mg p.o. in the morning and 500 mg at night for 1 week, and was again increased to 1000 mg b.i.d. Also included in the treatment plan was a referral to Ophthalmology and regular blood and liver lab tests.
Excisional Biopsy
The two biopsies were read by Dr. Oda and Dr. Morton of the Oral Pathology Biopsy Service at the University of Washington. The first biopsy was submitted in formalin for H & E staining and the second biopsy was submitted in transport medium for direct immunofluorescence staining. The latter biopsy was read by Dr. Morton and was the more specific of the two specimens. The direct immunofluorescence antibody staining was positive for IgG (Figure 7) and C3 (Figure 8) antibodies and was also focally positive with antibodies to fibrinogen. The positive IgG and C3 staining was pericellular and intracellular, involving the epithelial cells above the basal cell layers. The H & E stained frozen section (Figures 5 & 6) showed evidence of a split above the basal cell layer as well as areas of acantholysis. The connective tissue was infiltrated by lymphocytes, plasma cells, and neutrophils.
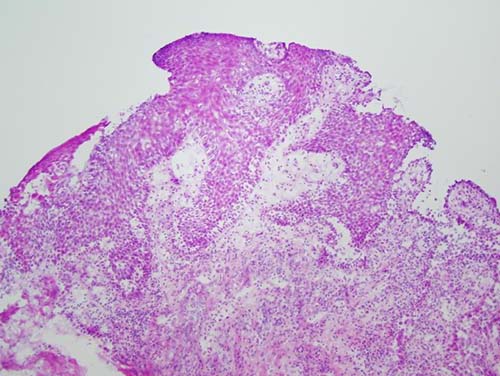
Figure 5. Low power (x100) Histology view of the H & E stained frozen section demonstrating a small punch biopsy with supra basilar epithelial split and inflamed underlying connective tissue.
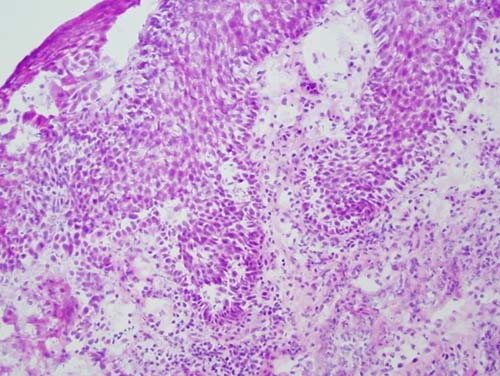
Figure 6. Low power (x200) Histology view of the H & E stained frozen section demonstrating a small punch biopsy with supra basilar epithelial split and mild acantholysis of the middle spinous layer.
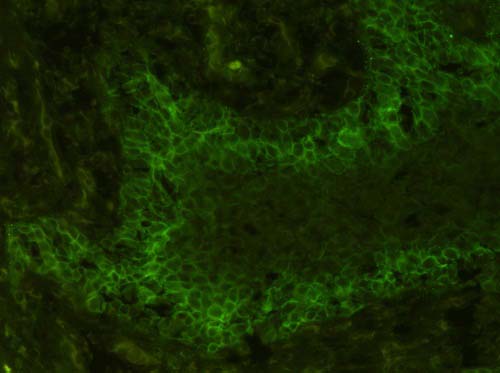
Figure 7. Low power (x200) view of a direct immunofluorescent stain demonstrating positive staining with C3 antibody with a chicken wire intercellular deposits in the deep spinous layer.
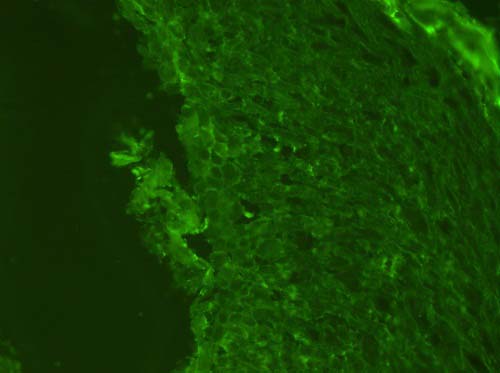
Figure 8. Low power (x200) view of a direct Immunoflourescent stain demonstrating mildly positive staining with IgG antibody with a chicken wire intercellular deposits between the spinous layer cells.
After you have finished reviewing the available diagnostic information