Well-defined and large radiolucency left ramus and condyle
Can you make the correct diagnosis?
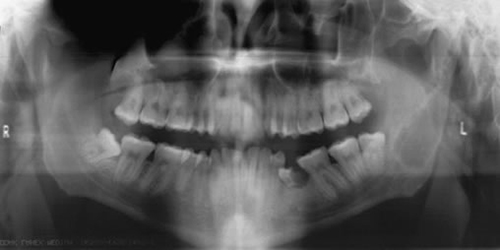
This is a 22-year-old Alaska Native male with history of 120 pounds of weight loss. He presented to Seattle Indian Health Board clinic for a routine dental visit. The head and neck examination was within normal limits. There is was no evidence of facial swelling or asymmetry or bony expansion. However, the panoramic radiograph (Figure 1) revealed a large, well-defined and corticated unilocular radiolucency of the left ramus extending and involving the condylar process and condylar head. The radiolucency of the condyle is multilocular.
Sorry! you are incorrect
Although the radiographic findings can be supportive of traumatic bone cavity, the location (ramus and condyle) are rare locations. The histology was not supportive of TBC.
The jawbones are subject to cyst-like or pseudocyst structures such as the salivary gland depression and traumatic bone cavity. Traumatic bone cyst is best called traumatic bone cavity since this condition does not represent a true cyst. Traumatic bone cavity (TBC) is not unique to the jawbones; it is also described in the long bones and is known as a simple solitary bone cyst or unicameral cyst (UBC) occurring mostly in the humerus or femur, close to the epiphyseal plate of children (1). The long bone simple cyst is similar to the jaw traumatic bone cavity radiographically and occurs in the same age range. Trauma has been suggested as the etiology along with other non-substantiated theories such as cystic degeneration of a preexisting tumor or of the fatty marrow in the area. The latter theory is just that without any scientific evidence to support it.
Some reports suggest that it is more common in males (2) while others report equal distribution between males and females (1). The long bone counterpart is more common in males by a ratio of 2.5:1. Most reports agree that the average age of occurrence is below 20 years of age (1-2). These lesions can occur, but are uncommon, over the age of 30. Kaugars reported a higher number of traumatic bone cavity in African American females compared to the literature (1). The latter patients were over the age of 30 (1-2). This may suggest an association with florid cemento-osseous dysplasia. In the mouth, mandible is the most commonly affected area, where over 95% of the cases occur, especially in the posterior premolar-molar area. They rarely extend to the ramus; therefore this case would be unique in that it extends very high into the ramus. Also, TBC are known to cross the midline anteriorly. In one study, 27% were anterior to the canine and some crossed the midline. They are usually unilocular and radiolucent, typically above the alveolar canal and in many cases with a scalloped superior border spreading between the roots of teeth. The latter are vital and are frequently found hanging within the empty cavity. About 25% of the lesions present in the anterior mandible apical to the canine tooth and usually are round and unilocular, which can be mistaken for a periapical lesion leading to an unnecessary endodontic treatment. Therefore, it is important to test the vitality of the teeth and carefully examine the radiographs for changes consistent with a periapical granuloma or cyst. Large, expansile and multilocular traumatic bone cavities (as is the case in the condyle of this patient) have been described, but are rare. Expansion is not characteristic of TBC but it is described in about 26% of the cases (1). They are otherwise asymptomatic. The margins of these lesions range from very well defined to corticated to punched out. Pathologic fractures associated with traumatic bone cavity have been described in the jaws, but are rare. They are however more common with those of the long bones.
Clinically, surgeons report an empty cavity at entrance in about two thirds of the cases and straw-colored fluid filled cavities in about one third of the cases. Blood clot is also present occasionally. The bony cavity is scraped to generate bleeding, which is considered the treatment of choice for this condition. Other methods of treatment have been tried, such as packing the curetted cavity with autogenous blood, autogenous bone and hydroxyapatite (2). Various other reports demonstrate healing of traumatic bone cavity after injection of autogenous blood, after aspiration and after endodontic treatment. These lesions may spontaneously heal, but rarely. Biopsy material consists of fragments of viable bone and loose connective tissue, as reported in our case. Osteoclast-like giant cells have also been described in a few cases (1-2). Exploration surgery usually leads to healing. Recurrence is rare.
Sorry! you are incorrect
The large radiolucency extending posteriorly into the ramus is consistent with the clinical behavior of an OKC but the histology is not supportive of it, no is the involvement of the condyle.
The Odontogenic keratocyst is an aggressive odontogenic cyst, known for its rapid growth and its tendency to invade the adjacent tissues, including bone. It has a high recurrence rate and is associated with basal cell nevus syndrome. It affects patients in the age ranges of 20-29 and 40-59, but cases in patients ranging in age from 5 to 80 years have been reported (3). The distribution between sexes varies from equal distribution to a male-to-female ratio of 1.6:1, except in children. Odontogenic keratocysts may occur in any part of the upper and lower jaw, with the majority (almost 70%) occurring in the mandible. They occur most commonly in the angle of the mandible and ramus (4). Radiographically, OKCs present predominantly as unilocular radiolucencies with well-defined or sclerotic borders; they may also present as multilocular radiolucencies, but rarely. OKCs commonly present as unilocular radiolucency with scalloped borders. Teeth associated with OKC are vital. OKCs grow to sizes larger than any other odontogenic cysts. They usually penetrate the bone rather than expand it and grow in an anterior to posterior direction (3-4). Despite this aggressive growth, they often remain asymptomatic, thus growing to large sizes and hollowing the bone. Treatment of choice is surgery with cauterization especially with Carnoy’s solution.
Sorry! you are incorrect
The location and focal multilocular appearance is consistent with ameloblastoma. The lack of facial expansion is not supportive of it; neither is the histology.
Ameloblastoma is one of the most common benign neoplasms of odontogenic origin. It accounts for 11% of all Odontogenic neoplasms/hamartomas (5-6). It is a slow-growing, persistent, and locally aggressive neoplasm of epithelial origin. It affects a wide range of age distribution but is mostly a disease of adults, at an average age of 33, with equal sex distribution. Reports from Africa and India show male predilection.
Almost 85% of ameloblastomas occur in the posterior mandible, most in the molar-ramus area, some in the anterior mandible. About 15% occur in the maxilla, the vast majority in the posterior maxilla. Solid ameloblastoma is characteristically expansile, radiolucent and multilocular in nature. It can however be unilocular and associated with impacted teeth resembling a dentigerous cyst and is known as cystic (unicystic) ameloblastoma. Cystic ameloblastomas are less aggressive than the multilocular solid counterpart. Ameloblastomas, if not treated, can reach very large sizes with facial disfiguring. They loosen, displace and resorb adjacent teeth. With the exception of jaw expansion, it is usually asymptomatic unless infected where it can be mildly painful. Parasthesia, anesthesia is extremely rare, unless they are very large in size. Also, ameloblastomas tend to expand rather than perforate the cortical bone. If the later occurs with extension into the adjacent soft tissue, it would have a higher tendency for recurrence and therefore would have a worse prognosis than those completely encased by bone (5-6).
Three clinical types of ameloblastoma are described: solid (multilocular), cystic (unilocular) and peripheral (gingival soft tissue). The solid type is treated with resection or en bloc. Resected jaws may require secondary reconstruction (7). Cystic are treated with thorough curettage while peripheral are treated with conservative surgical removal.
Congratulations! You are correct
It is obvious that the diagnosis of benign fibro-osseous lesion implies that more than one fibro-osseous lesion was considered. Based on the histology of this case, fibrous dysplasia (FD) and central ossifying fibroma (COF) were considered and fibrous dysplasia was favored not just based on the histology but on the radiographical, clinical and surgical presentation.
Mandibular ramus and the condyle are unusual locations for fibrous dysplasia or central ossifying fibroma, more so for COF. The histology is however most consistent with fibrous dysplasia given the lack of osteoblasts, the curvilinear bony trabeculae and the artifactual retraction from the connective tissue from the bony trabeculae. The clinical presentation of no expansion facially and moderate expansion lingually is not typical of either FD or COF since both tend to be expansile. It is especially unusual for central ossifying fibroma not to be expansile. The gritty consistency described by the surgeon is more consistent with FD.
The etiology of fibrous dysplasia is unknown. The monostotic (one bone or bone complex area) form constitutes approximately 80% of all fibrous dysplasia cases while the polyostotic affects one or more bones with multiple lesions (8). However, FDs are expansile and disfiguring lesions, whether single or multiple, which differentiate them from the usually flat osteomas of Gardner’s syndrome. Monostotic FD, which involves the jaws, affects males and females equally. It occurs in childhood and at puberty and usually stops growing at age 30. It appears as an asymptomatic swelling of the maxilla or mandible; the maxillary lesion is the most common. It may involve bones other than the maxilla, including the zygoma, sphenoid and others. It is usually unilateral and is known to displace the teeth, but otherwise is firmly seated (8-10). The growth is usually slow, but rapid growth has been described, especially during puberty. The radiographic appearance, especially of the maxilla, is classically described as a ground glass appearance where fine radiopacity is noted. The mandibular lesions are much more deceptive because they tend to vary more, thus making diagnosis with a radiograph difficult. They range from cystic unilocular radiolucency to multilocular radiolucency to the classical ground glass radio-opacity (9-10).
Polyostotic fibrous dysplasia constitutes approximately 20% of FD cases (9). Two principle sub-types are described; Jaffe’s and Albright’s syndrome. The latter represents the more severe form with endocrine disturbances (precocious puberty in females). Polyostotic FD is more common in females than males (8-10). Multiple bones are affected including long bones in addition to the jawbones. The clinical presentation depends on the type. Albright’s is associated with hormonal changes, including precocious puberty and cafe au lait spots. Jaffe’s has multiple bones with FD and cafe au lait spots but no hormonal changes. Treatment may be necessary and is preferably performed after cessation of growth due to the high incidence of re-growth and requirement for secondary procedures. The surgeons decided against treatment and opted to keep the patient on close observation. Radiation therapy is contraindicated since significant incidence of development of osteosarcoma in the irradiated bone has been documented. Malignancies such as osteosarcoma arising in an area of FD that has not been irradiated have been described, but rarely; these occur mainly in irradiated lesions. The overall prognosis of this patient is good with close follow-up visits.
References
- Kaugars GE, Cale AE. Traumatic bone cyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1987; 63: 318-324.
- Dellinger TM, Holder R et al. Alternative treatments for a traumatic bone cyst: a longitudinal case report. Quintessence Int. 1998; 29: 497-502.
- Shear M. Odontogenic keratocysts: natural history and immunohistochemistry. Oral Maxillofacial Surg Clin N Am. 2003; 15: 347-362.
- Oda D, Rivera V et al. Odontogenic keratocyst: the northwestern USA experience. J Contemp Dent Pract. 2000 Feb 15; 1(2): 60-74.
- Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol 1995;31B:86–99.
- Adekeye EO, McLavery K. Recurrent ameloblastoma of the maxillofacial region. Clinical
features and treatment. J Maxillofac Surg 1986;14:153-157. - Gardner DG. Some current concepts on the pathology of ameloblastomas. J Oral Maxillofac Surg 1996;82:660-669.
- Parekh SG, Donthineni-Rao R et al. Fibrous Dysplasia. J Am Acad Orthop Surg. 2004;12:305-313.
- Tsai EC, Santoreneos S et al. Tumors of the skull base in children: review of tumor types and management strategies. Neurosurg Focus. 2002: 15;12(5).
- Zacharin M. Paediatric management of endocrine complications in McCune-Albright syndrome. J Pediatr Endocrinol Metab. 2005;18:33-41.