Destructive Soft Tissue Lesion, Right Posterior Maxilla
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Drs. Preston Gomez and Thomas Dodson
University of Washington, Oral & Maxillofacial Surgery, Seattle WA
Case Summary and Diagnostic Information

This is a 65-year-old female referred by her dentist to the Department of Oral & Maxillofacial Surgery at the University of Washington for evaluation of a growing lesion in the right posterior maxilla.
Diagnostic Information Available
This is a 65-year-old female referred by her dentist to the Department of Oral & Maxillofacial Surgery at the University of Washington for evaluation of a growing lesion in the right posterior maxilla (Figures 1 & 2). The lesion had been present since late October 2013. She described a roughly eight-year history of painful flare-ups that would subside on their own after a few days. However, since October 2013, the posterior maxilla had developed another such flare-up which had not healed. She described dull pain, and there was a loose molar tooth (Figure 2). The area was unsuccessfully treated with antibiotics. She reported no paresthesia.

Figure 1 This is a clinical photograph taken at the first clinical presentation; note the ulcerated, deeply infiltrative bony lesion in the right posterior maxilla. Also, note the buccal bony expansion.
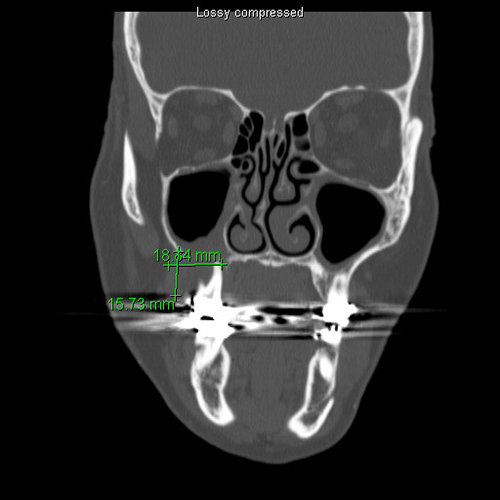
Figure 2 This is a CT scan taken at the first clinical presentation; note the large, destructive, ill-defined radiolucent lesion involving the right posterior maxillary alveolar ridge causing resorption and mobility of teeth #s 2 & 3.
The patient’s past medical history is significant for diverticulitis requiring colostomy followed by reconnection. The past medical history is negative for tobacco use, however the patient has 6-10 alcoholic beverages per week on average.
The patient reported multiple painful flare-ups in the area over many years. However, the current lesion (Figure 1) started in October and did not heal. It was destructive, causing tooth mobility, an observation supported by the radiographic images (panoramic and CT scan). The panoramic radiograph (not shown) and the CT scan (Figure 2) show an ill-defined radiolucent lesion in the right posterior maxilla with thickening of the maxillary sinus and root resorption of teeth #s 2 & 3.

Figure 1 This is a clinical photograph taken at the first clinical presentation; note the ulcerated, deeply infiltrative bony lesion in the right posterior maxilla. Also, note the buccal bony expansion.
Figure 2 This is a CT scan taken at the first clinical presentation; note the large, destructive, ill-defined radiolucent lesion involving the right posterior maxillary alveolar ridge causing resorption and mobility of teeth #s 2 & 3.
Treatment
Under local anesthesia, an incisional biopsy was performed. Based on the biopsy results, the lesion was completely excised under general anesthesia.
Excisional Biopsy
Histologic examination reveals multiple pieces of soft tissue composed of an infiltrative neoplasm with biphasic cellular morphology. In some areas, the neoplasm is arranged in elongated bundles of spindle-shaped cells that are crisscrossing each other (Figure 3). These cells are positive with immunohistochemistry stain for pancytokeratin Oscar (Figure 4). Most other fragments show evidence of spindle-shaped cells associated with more epithelioid cells that are haphazardly arranged and are positive with antibodies to both pancytokeratins AE1/AE3 (Figure 5 & 6). The cells show high-grade cellular and nuclear pleomorphism (Figure 5). They show evidence of many mitotic figures, some of which are atypical. There is evidence of very large and hyperchromatic nuclei. There is evidence of large cells with prominent nucleoli. Keratin formation is not identified.
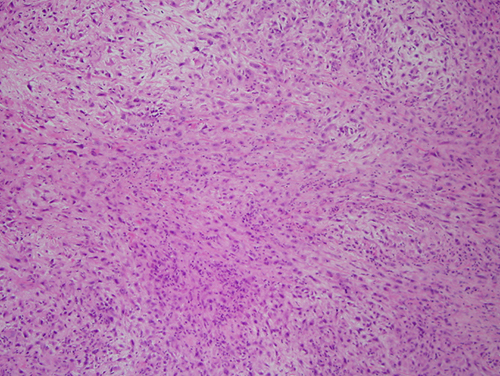
Figure 3 Low power (x40) H & E histology demonstrates an infiltrative neoplasm with biphasic cellular morphology. In this view most of the neoplastic cells are arranged in elongated bundles of spindle-shaped cells that are crisscrossing each.
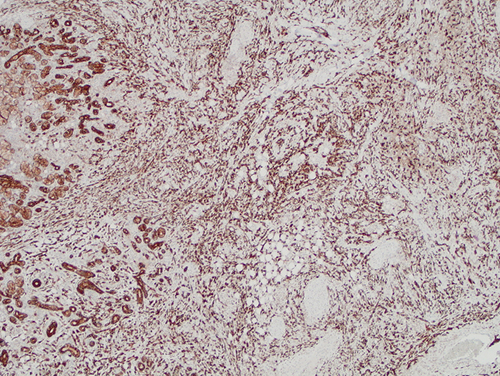
Figure 4 Higher power (x100) immunohistochemistry stain with antibody to pancytokeratins (Oscar) demonstrates strong positive staining of all neoplastic cells and some normal internal positive control representing the minor salivary gland tissue. Most of the neoplastic cells in this view are spindle-shaped in morphology.
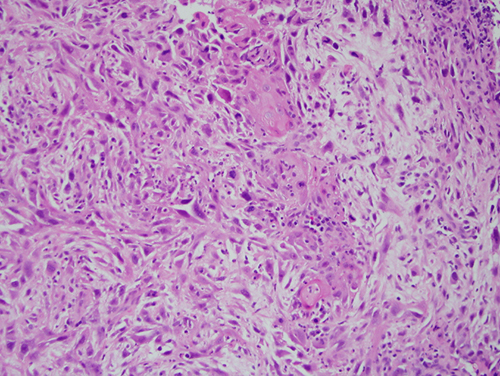
Figure 5 Higher power (x200) H & E histology demonstrates sheets of neoplastic cells with high-grade nuclear and cellular pleomorphism. In focal areas, the cells have epithelioid cytoplasmic morphology.
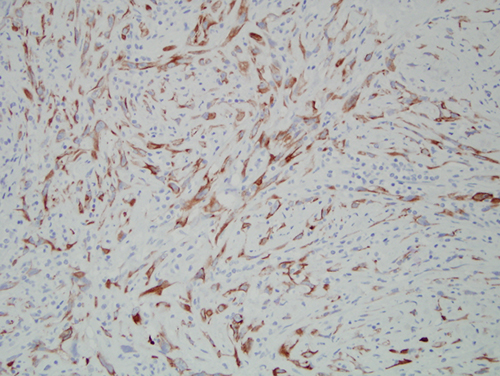
Figure 6 Higher power (x200) immunohistochemistry stain of the more epithelioid neoplastic cells stained with antibody to pancytokeratins AE1/AE3 which is positive.
After you have finished reviewing the available diagnostic information