All cases are discussed by: Dr. Dolphine Oda, UW-Oral Pathology Biopsy Service
Large unilocular radiolucency left posterior mandible
Contributed by: Dr. Randall Eggert
Oral & Maxillofacial Surgery, Redmond, Washington
Case Summary and Diagnostic Information
This is a 25-year-old female who was referred by her general dentist for the evaluation of a large asymptomatic lytic lesion in the left posterior mandible.
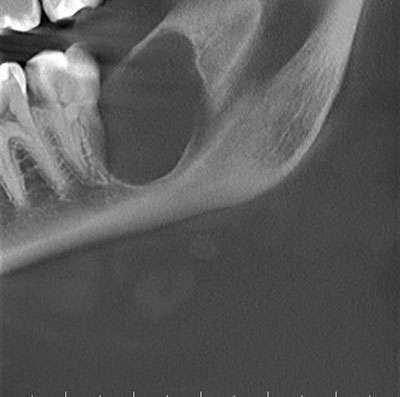
This is a 25-year-old female who was referred by her general dentist for the evaluation of a large asymptomatic lytic lesion in the left posterior mandible. This lesion was located distal to tooth #18 and in area of previously extracted tooth #17. The radiographic findings show a unilocular and corticated radiolucency in the posterior mandible (Figure 1). The CBCT shows an expansile lesion, thinning the lingual bone. Tooth #18 shows no evidence of resorption but is slightly pushed mesially. The lesion is of unknown duration and measures approximately 17x16x11mm in size. The soft tissue overlying this lesion was intact and normal in appearance. No cortical expansion was detected clinically and no paresthesia was present.
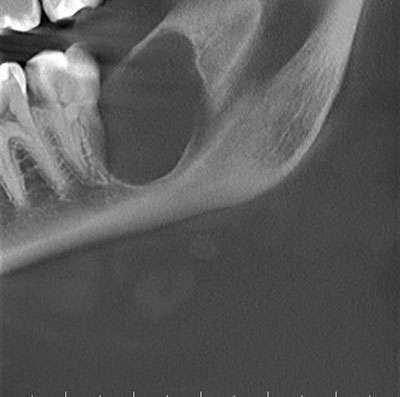
Figure 1 This is a partial image of a panoramic view from a CBCT image taken at first clinical presentation demonstrating a large unilocular and corticated radiolucency of the left posterior mandible-area distal to tooth #18.
The patient’s past medical history was unremarkable. She was not on any medications and had no allergies to report.
The partial panoramic view of the CBCT (Figure 1) shows a corticated and unilocular radiolucency posterior to tooth #18. The coronal view of the CBCT (Figure 2) shows mild expansion, more so lingually and also shows thinning of the lingual cortical bone but no frank perforation is noted. The axial view of the CBCT (Figure 3) shows the same lesion from a different angle. Tooth #18 is vital and is not mobile. It does not show resorption.
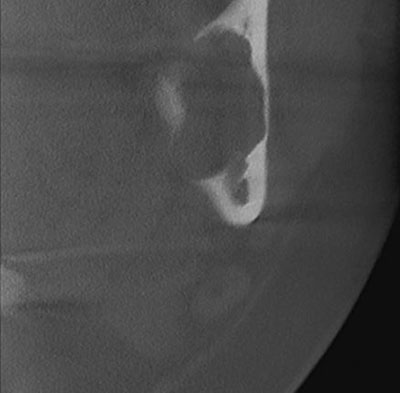
Figure 2 This is a partial image of a coronal view of the CBCT taken at first clinical presentation demonstrating mild expansion. The expansion is more lingually. This image also shows thinning of the lingual cortical bone but no frank perforation is noted.

Figure 3 This is a partial image of an axial view of the CBCT taken at first clinical presentation demonstrating mild expansion, more lingually but no frank perforation is noted.
Following the sedation of the patient and the application of local anesthesia, a full thickness mucoperiosteal flap was elevated. A dehiscence was noted in cortical bone distal to tooth #18. This was enlarged with rotatory instrumentation and the lesion was removed by curettage. It came out in friable, grey/brown clumps that were not tightly adherent to the walls of the cavity. Following removal, the cavity was irrigated with copious amounts of normal saline, a dressing was placed, and the flaps were re-approximated with 4- chromic gut sutures. The specimen was submitted for histopathological evaluation.
Histological examination revealed multiple large pieces of vascular and cellular granulation tissue with many giant cells and clusters of hemosiderin pigment (Figures 4-6). The giant cells were of variable shapes and sizes, some were arranged in whorls (Figure 5) but mostly were haphazardly arranged (Figure 6). The granulation tissue is vascular and cellular and contains extravasated erythrocytes and hemosiderin pigment (Figure 4-5).
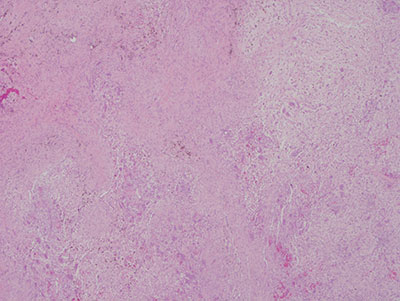
Figure 4 Low power (x40) H & E stained section demonstrating a mass of vascular and cellular granulation tissue with many multinucleated giant cells, clusters of hemosiderin pigment and extravasated erythrocytes.
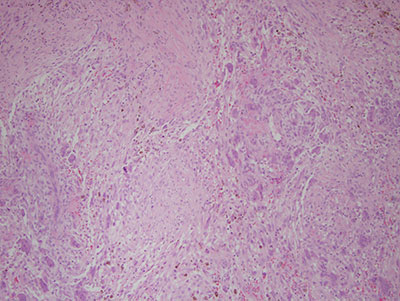
Figure 5 Higher power (x100) H & E stained section demonstrating many giant cells, some arranged whorls, cellular granulation tissue, hemosiderin pigment and extravasated erythrocyte.
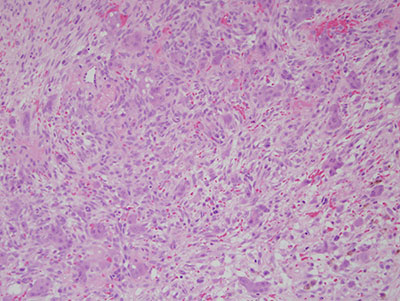
Figure 6 Higher power (x200) H & E stained section demonstrating many giant cells haphazardly arranged in cellular granulation tissue background containing extravasated erythrocyte.
After you have finished reviewing the available diagnostic information