Return to Case of the Month Archives
Multiple dark-brown oral macules
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Contributed by
Drs. Peter Van der Ven, Don Tran, and Zsolt Argenyi
Federal way Oral Medicine and University of Washington, School of Medicine
Case Summary and Diagnostic Information
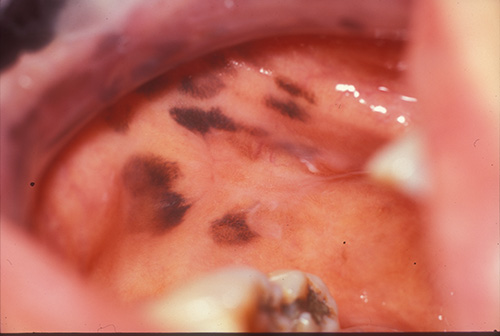
An 87-year-old non-smoking Asian woman presented with a three-year history of hyperpigmented macules on the buccal mucosa (Figure 1), tongue, maxillary edentulous alveolar ridge, hard and soft palate and lips. The macules are irregular, 4-8 mm in size and are dark brown to black in color. They are otherwise not palpable or indurated. The patient reports that they were first noticed three years ago and that they have increased in number over time.
Diagnostic Information Available
An 87-year-old non-smoking Asian woman presented with a three-year history of hyperpigmented macules on the buccal mucosa (Figure 1), tongue, maxillary edentulous alveolar ridge, hard and soft palate and lips. The macules are irregular, 4-8 mm in size and are dark brown to black in color. They are otherwise not palpable or indurated. The patient reports that they were first noticed three years ago and that they have increased in number over time.
Figure 1 This is a photograph representing the buccal mucosa with multiple darkly pigmented macules. Note the lack of uniformity in color as well as in shape and size.
The patient is generally in good health and is negative for malignant melanoma, adrenal insufficiency or familial polyposis. Her history is also negative for tobacco or alcohol use. Her medications include Norvasc, Atenolol, Synthroid, iron supplements, multivitamin, baby aspirin, calcium/vitamin D and vitamin E supplements.
The patient has dark brown to black, non-palpable, non-indurated oral macules, which involve the bilateral buccal, upper and lower oral labial, hard palate, and maxillary edentulous ridge gingival mucosal surfaces. The macules measure 4-8 mm in diameter with focal regions of confluence.
Treatment
Under local anesthesia two separate biopsies were performed. Based on the histology, no treatment was rendered. Close clinical follow-up was recommended.
Incisional and excisional biopsy
Both buccal mucosal biopsies demonstrated non-neoplastic stratified squamous epithelium with basal layer hyperpigmentation and increased deposition of dark-brown pigment granules predominantly in histiocytes and freely in the stromal matrix of the superficial lamina propria. The pigment granules were stained with a Fontana-Masson stain, but were negative for iron stain. Nevertheless, melanocytic hyperplasia was not appreciated by S100 and Melan-A immunohistochemical stains.
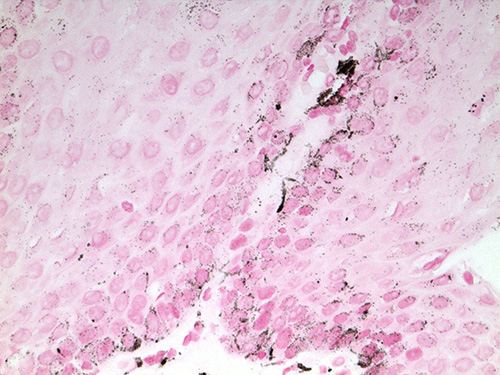
Figure 2 Low power (100X) H & E histology representative of both biopsies. The buccal mucosa demonstrates non-neoplastic epithelial hyperplasia with basal cell layer hyperpigmentation and increased deposition of dark-brown pigment granules in the superficial lamina propria.
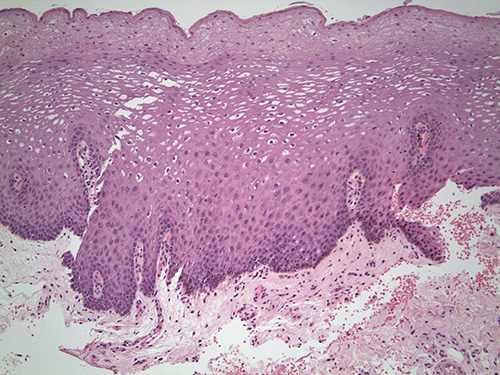
Figure 3 High power (400X) Fontana-Masson stain is positive for melanin pigment at the basal cell layer and superficial lamina propria. Dendritic pseudopods are identified in the basal and parabasal cell layers.
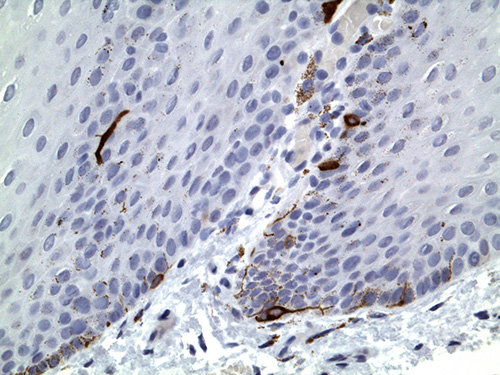
Figure 4 High power (400X) immunohistochemistry stain with Melan A is negative for melanocytic hyperplasia. Melanin pigment is present in the basal cell layer and superficial lamina propria. Similar morphology was identified with S100 protein antibody. Dendritic pseudopods are identified in the basal and parabasal cell layers.
After you have finished reviewing the available diagnostic information