Unilocular radiolucency between teeth #s 26 & 27
Contributed by Dr. Samuel Bobek
Oral & Maxillofacial Surgery, Seattle WA
Case Summary and Diagnostic Information

This is a 43-year-old white female who was referred to Dr. Bobek for the evaluation of a slowly growing swelling in the right anterior mandible.
This is a 43-year-old white female who was referred to Dr. Bobek for the evaluation of a slowly growing swelling in the right anterior mandible (Figure 1). A periapical radiographs shows a well-demarcated radiolucency with a hint of scalloping and multilocular appearance between teeth #s 26 & 27 (Figure 2). The patient noticed the swelling 2-3 months ago. She noticed a small change in her bite with movement of the lateral incisor. No symptoms otherwise – no pain, drainage, anesthesia or paresthesia.

Figure 1 This is an intra-oral photograph demonstrating a buccal swelling between teeth #s 26 & 27

Figure 2 This is a periapical radiographic view at first presentation demonstrating a well-demarcated, radiolucency with partial scalloped border and a hint of multilocular appearance between teeth #s 26 & 27. It is mildly displacing the teeth.
The past medical history is significant for malignant melanoma and hypothyroidism. Malignant melanoma was treated with surgical excision a few years ago. The patient is nonsmoker. She reports allergies to latex and amoxicillin.
The clinical examination revealed a soft nontender buccal swelling in the right anterior mandibular alveolar bone between teeth #s 26 and 27 (Figures 1 & 2). No other lesions were noted on examination. The periapical radiograph demonstrates a well-defined and partially corticated radiolucency with a hint of scalloped border and multilocular center. The cone beam CT showed erosions of the labial and lingual alveolar bone. Teeth #s 26 and 27 are pushed apart and are vital.
The procedure was performed under local anesthesia. A sulcular incision was made from the anterior mandible in order to expose the buccal bone. There was no buccal cortical bone and the lesion was found to solid in consistency. The grey soft tissue was sampled and sent for histologic evaluation. The surgical site was thoroughly irrigated and closed. 10 day postoperative visit demonstrated loosening of tooth 26 as well as tenderness. No drainage or numbness.
The incisional biopsy revealed a benign neoplasm of odontogenic epithelial origin made up of epithelial islands of variable shapes and sizes (Figures 3 and 4). The periphery of these islands is lined by one layer of palisaded cuboidal/columnar cells exhibiting focal areas of reversed polarization (Figures 3 and 4). The center of the islands is filled with squamous epithelial cells or stellate reticulum-type epithelial cells undergoing partial cystic degeneration (Figures 3 and 4). The surrounding connective tissue is fibrotic. Focally, thin cords of epithelial cells are present and lack the peripheral palisading (Figure 4).
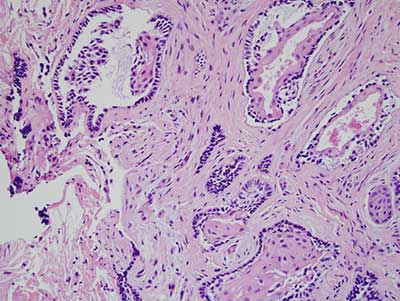
Figure 3 This is an H & E stained section at x 100 magnification demonstrating a neoplasm of odontogenic epithelial origin made up of islands surrounded by dense fibrous connective tissue. The epithelial islands are of various sizes and shapes and show cystic degeneration within the center of most islands. The periphery of each island is lined by a basal/columnar cell layer that is palisaded with focal reverse polarization of the nuclei. The epithelium layering the basal cells are spindle shaped with feature of stellate reticulum and squamous cells.
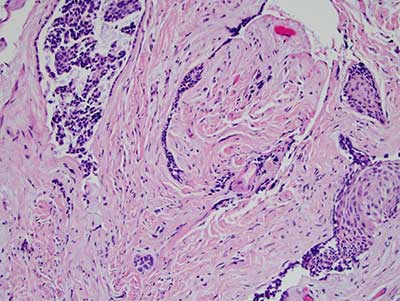
Figure 4 This is an H & E stained section at x 200 magnification demonstrating the cords and small islands of epithelial cells lacking the typical palisaded and polarized morphology surrounded by dense fibrous connective tissue.
After you have finished reviewing the available diagnostic information