Return to Case of the Month Archives
Recurrent large anterior mandibular unilocular radiolucency
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Contributed by
Dr. Robert Dixey
Bellevue Oral Surgery
Case Summary and Diagnostic Information

This is a 28-year-old Asian male of slender build. He first presented on August 8, 1990 with a large anterior mandibular expansion.
Diagnostic Information Available
This is a 28-year-old Asian male of slender build. He first presented on August 8, 1990 with a large anterior mandibular expansion. A panoramic radiograph (Fig 1) demonstrated a large, well defined unilocular radiolucency in the anterior mandible between teeth #s 22 and 28. This lesion was expansile and was displacing and resorbing teeth; it was otherwise not painful and the patient was not aware of its duration. Previous radiographs were not available for review. Despite thorough curettage, this lesion recurred in 1992 and again in 2005. The patient is in good general health, has no allergies and is not taking any medications. The lesion has not caused him any pain to date.

The patient is otherwise in good general health. He has no allergies and is not taking any medications.
Physical examination revealed an expansile lesion in the anterior mandible between teeth #s 22 and 28 (Fig 1). Panoramic radiographs showed a large, expansile, well demarcated to corticated unilocular radiolucency (Fig 1). This lesion recurred in 1992 after thorough curettage of the area. The first recurrence (Fig 2) was small and well demarcated between teeth #s 28 and 29, but less well defined in area of missing teeth #s 26-27. This lesion was also thoroughly curetted and several teeth were extracted (teeth #s 22-24 and 28-30). The second recurrence (Fig 3) took place in 2005, 13 years after the first recurrence. It was mostly in the anterior mandible and was a well demarcated to corticated unilocular radiolucency. It was also slightly expansile.

Figure 1. Panoramic view of the primary tumor taken in 1990 demonstrating a large unilocular and corticated radiolucency involving the area of teeth #s 22-28.

Figure 2. Panoramic view of the first recurrence taken in 1992. Note the unilocular radiolucency between teeth #s 28 and 29 and less defined between teeth #s 26 and 27.

Figure 3. Panoramic view of the first recurrence taken in 1992. Note the unilocular radiolucency between teeth #s 28 and 29 and less defined between teeth #s 26 and 27.
The histology of all three specimens was consistent; the primary lesion was more solid than the second recurrence, in which a combination of cystic and solid components were identified (Figs 4-5). Overall, the three specimens were made up of small islands of epithelial cells of various shapes and sizes. The islands were made up of small and uniform basaloid cells with round and hyperchromatic nuclei and scanty cytoplasm (Fig 4) intermixed with ghost cells. The latter were much less evident in the last recurrence. Many mitotic figures were present in the last recurrence (Fig 6) which may indicate a progressively more aggressive behavior.
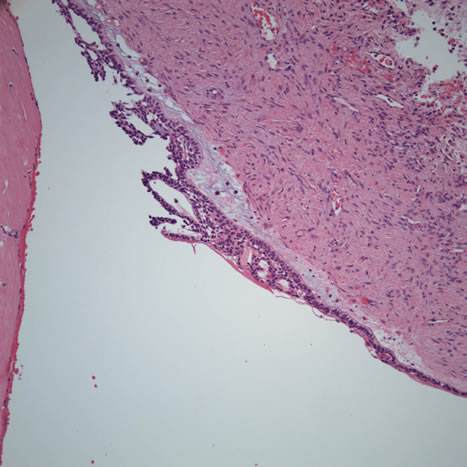
Figure 4. Low power (x100) histology shows a cystic structure with lining epithelium with ameloblastoma-like morphology. Ghost cells were sparse to absent in this specimen (representing the second recurrence) but were abundant in the specimens from the primary and first recurrence.
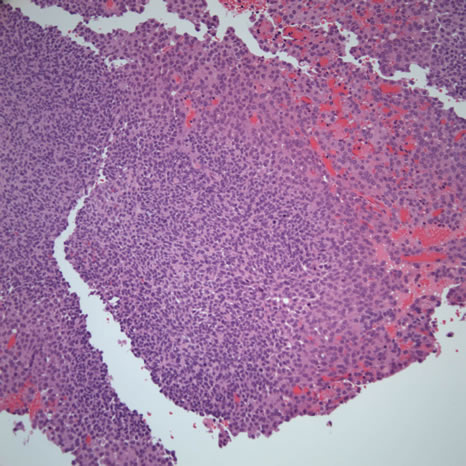
Figure 5. Low power (x100) histology shows the more solid component of this tumor. Sheets of small and uniformly basaloid epithelial cells are present.
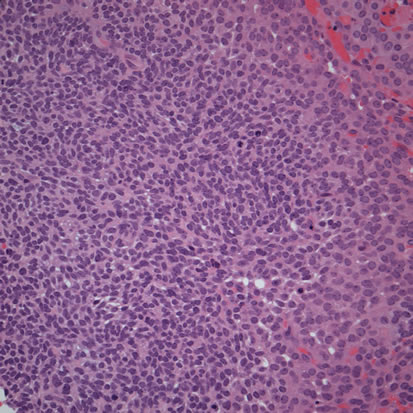
Figure 6. High power (x200) histology shows sheets of small and uniformly basaloid epithelial cells with high mitotic activity.
After you have finished reviewing the available diagnostic information