Large radiolucency left maxilla and left maxillary sinus
Can you make the correct diagnosis?
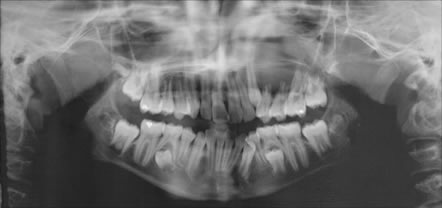
This is a 12-year-old Hispanic girl who was referred by her general dentist for a large swelling in the left maxilla. It involved teeth #s 11-15 and the maxillary sinus (Figure 1). The lesion was of unknown duration and was 2 x 4 cm in size. The soft tissue overlying the lesion was reddish in color and the swelling was both buccal and palatal. Teeth #s 12-14 were mobile. The CT scan showed the tumor to have infiltrated the roots of the left maxillary permanent dentition. Her past medical history is unremarkable.
Sorry! you are incorrect
Odontogenic keratocysts can be large and destructive but would not cause a gross jaw expansion as described in this patient. It nonetheless should be considered on the differential diagnosis. The histology in this case was not supportive of OKC.
The Odontogenic keratocyst is an aggressive odontogenic cyst, known for its rapid growth and its tendency to invade the adjacent tissues, including bone. It has a high recurrence rate and is associated with basal cell nevus syndrome. It affects patients in the age ranges of 20-29 and 40-59, but cases in patients ranging in age from 5 to 80 years have been reported (1). The distribution between sexes varies from equal distribution to a male-to-female ratio of 1.6:1, except in children. Odontogenic keratocysts may occur in any part of the upper and lower jaw, with the majority (almost 70%) occurring in the mandible. They occur most commonly in the angle of the mandible and ramus (2). Radiographically, OKCs present predominantly as unilocular radiolucencies with well-defined or sclerotic borders; they may also present as multilocular radiolucencies, but rarely. OKCs commonly present as a unilocular radiolucency with scalloped borders. Teeth associated with OKC are vital. OKCs grow to sizes larger than any other odontogenic cysts. They usually penetrate the bone rather than expand it and grow in an anterior to posterior direction (1-2). Despite this aggressive growth, they often remain asymptomatic, thus growing to large sizes and hollowing the bone. Treatment of choice is surgery with cauterization, especially with Carnoy’s solution.
Sorry! you are incorrect
The location of occurrence in the maxilla, the age of this patient and the expansion accompanying the tumor are all factors in support of a diagnosis of fibrous dysplasia (FD). Although FD of the maxilla tends to be more “ground glass” and blends in with the surrounding tissue, a well demarcated unilocular radiolucency can also fit the spectrum of the radiographic presentation of FD. The histology in this case, however, does not support a diagnosis of FD.
Monostotic (one bone or bone complex) FD constitutes approximately 80% of all fibrous dysplasia cases while the polyostotic affects one or more bones with multiple lesions (9). Fibrous dysplasia is an expansile and disfiguring lesion and affects males and females equally. It occurs in childhood and at puberty and usually stops growing at age 30. It appears as an asymptomatic swelling of the maxilla or mandible; maxilla being the more common. It may involve bones other than the maxilla, including the zygoma, sphenoid and others. It is usually unilateral and is known to displace the teeth, but otherwise is firmly seated (9-10). The growth is usually slow, but rapid growth has been described, especially during puberty. The radiographic appearance, especially of the maxilla, is classically described as a ground glass appearance where fine radiopacity is noted. The mandibular lesions are much more deceptive because they tend to vary more, thus making diagnosis with a radiograph difficult. They range from cystic unilocular radiolucency to multilocular radiolucency to the classical ground glass radio-opacity (9-11).
Treatment may be necessary and is preferably performed after cessation of growth due to the high incidence of re-growth and requirement for secondary procedures. Radiation therapy is contraindicated since significant incidence of development of osteosarcoma in the irradiated bone has been documented. Malignancies such as osteosarcoma arising in an area of FD that has not been irradiated have been described, but rarely.
Sorry! you are incorrect
The clinical presentation can be consistent with odontogenic neoplasms such as ameloblastoma, odontogenic myxoma, calcifying epidermal odontogenic tumor and others. This patient is on the low age range of cystic ameloblastoma but her age is not supportive of solid type of ameloblastoma or of odontogenic myxoma or Pindborg tumor. The histology in this case is not supportive of any odontogenic neoplasm (3-7).
Several odontogenic neoplasms are more common in children; these include adenomatoid odontogenic tumor (AOT), ameloblastic fibroma (AF), ameloblastic fibro-odontoma (AFO), odontoma and cystic ameloblastoma. Children are much less likely to develop solid ameloblastoma, odontogenic myxoma or Pindborg tumor.
Adenomatoid odontogenic tumor is an uncommon benign epithelial odontogenic neoplasm; it most commonly occurs in the anterior maxilla in association with impacted lateral or canine in about 75% of cases. It occurs twice as commonly in the anterior maxilla with a 2:1 female predilection and an age range of 10-18 (3-6). It usually presents as a unilocular radiolucency, sometimes with flecks of radiopaque material resembling a dentigerous cyst (3).
Ameloblastic fibroma is a true neoplasm of mixed odontogenic tissue origin; it is more common in the mandible, molar area (70%), and usually occurs in young patients in the first and second decade. It is a slow growing lesion that can reach large sizes if untreated (3-6). It presents either as a unilocular or a multilocular radiolucency associated with impacted teeth (4).
Ameloblastic fibro-odontoma is a benign odontogenic neoplasm of mixed ectodermal and mesenchymal origin, occurring in patients around 10 years of age, with equal gender predilection. It is equally distributed between maxilla and mandible and is often associated with impacted teeth (3-6). This lesion presents as a well-circumscribed, expansile radiolucency with radiopaque material (5). It can reach large sizes.
Odontoma is one of the most common odontogenic lesions. It is of mixed ectodermal and mesenchymal origin and is usually associated with impacted teeth. It can occur at any age in the first two decades but is most common at an average age of 14 (3-6). It is slightly more common in the maxilla. It presents as a well-circumscribed radiolucency with one or more pieces of radiopaque material which resemble small teeth (6).
Cystic ameloblastoma is less aggressive than the classical solid/multilocular ameloblastoma (7-8). It usually occurs in young people; diagnoses begin in the first decade of life and about 50% of cases are diagnosed during the second decade, with an average age of occurrence of 14.3 in Africa and 14.7 in the USA (7). More than 90% of cases are described in the posterior mandible in association with an impacted third molar resembling a dentigerous cyst. In about 10% of the cases, it presents as unilocular radiolucency between or below the apex of teeth.
Congratulations! You are correct
Jaffe first coined the term “reparative” for central giant cell granuloma (CGCG). Most pathologists have since dropped the term “reparative” for lack of evidence that the pathogenesis is a reparative process. CGCG is described as a non-neoplastic process and yet can behave in a very aggressive and expansile manner, destroying bone and displacing teeth. Over 60% of CGCG cases occur in patients younger than 30 years of age, with twice as many occurrences in females as in males. CGCG is classified into aggressive and non-aggressive types; the aggressive type tends to occur in younger patients and causes disfiguration, especially after surgery. Over 70% of cases occur in the mandible anterior to the first molar tooth. This lesion has also been described in other cranio-facial and small long bones such as those of the hands and feet (12, 13).
The usual treatment for CGCG is surgery, ranging from curettage and en bloc to resection (13). The latter is used in aggressive and recurring cases (13). In the past ten years or so, alternatives to surgery have emerged with successful results, saving some patients from facial disfigurement. The most commonly used alternatives are: steroid injections (14), the most successful alternative treatment thus far, which require injections weekly or every 2-3 weeks, have no known side effects (even in children), and are the least expensive alternative treatment; calcitonin injections or nasal spray (15), which require daily injections or a nasal spray of salmon calcitonin for about a year and are safe for pregnant females; and interferon alfa-2a injections (16), which are administered 2-3 times per week for several months and are the most expensive alternative treatment.
A report by Carlos and Sedano (14) from Guatemala presented four patients with large CGCG cases treated with steroid injections. They demonstrated that regular steroid injections led to remarkable responses in all four patients without any side effects. All four patients had initial biopsies confirming the histological diagnosis of CGCG and had endocrine testing to rule out hyperparathyroidism. Two were pediatric patients, two-and-a-half and six years of age, with large lesions of the mandible and maxilla, respectively; they responded more rapidly to steroid injections than did the other two patients, who were adults of 31 and 34 years of age with large lesions of the maxilla and mandible, respectively. Injections were administered every two to three weeks. Complete healing, with small residual radiolucency requiring no further treatment, was noted in three patients; one patient, the six-year-old boy, had a maxillary swelling that was reduced from 5 cm in size to only 0.5 cm after four injections. The surgical specimen from the six-year-old consisted of fibrocollagenous stroma with few giant cells in comparison to the original biopsy, which consisted of loose and vascular granulation tissue with many giant cells. Fibrocollagenous stroma, with or without giant cells, has been described in association with both calcitonin and steroid treatment (14-15). There was no evidence of recurrence in these patients after 2-7 years of follow-up, nor were there any steroid-related complications in any of the patients. One must keep in mind that this report involves a very small number of cases; few firm conclusions can be reached, but the results are remarkable and show a more favorable outcome than surgical intervention, particularly in large and aggressively behaving pediatric cases.
References
- Shear M. Odontogenic keratocysts: natural history and immunohistochemistry. Oral Maxillofacial Surg Clin N Am. 2003; 15: 347-362.
- Oda D, Rivera V et al. Odontogenic keratocyst: the northwestern USA experience. J Contemp Dent Pract. 2000 Feb 15; 1(2): 60-74.
- Batra P, Prasad S, Parkash H. Adenomatoid odontogenic tumour: review and case report. J Can Dent Assoc. 2005 Apr;71(4):250-253.
- Chen Y, Li TJ, Gao Y, Yu SF. Ameloblastic fibroma and related lesions: a clinicopathologic study with reference to their nature and interrelationship. J Oral Pathol Med. 2005 Nov;34(10):588-95.
- Zouhary KJ, Said-Al-Naief N, Waite PD. Ameloblastic fibro-odontoma: expansile mixed radiolucent lesion in the posterior maxilla: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Oct;106(4):e15-21.
- de Oliveira BH, Campos V, Marçal S. Compound odontoma–diagnosis and treatment: three case reports. Pediatr Dent. 2001 Mar-Apr;23(2):151-7.
- Ord RA, Blanchaert RH,Nikitakis NG Sauk JJ. Ameloblastoma in children. J oral Maxillofacial Surg. 2002; 60: 762-770
- Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol 1995;31B:86–99.
- Parekh SG, Donthineni-Rao R et al. Fibrous Dysplasia. J Am Acad Orthop Surg. 2004;12:305-313.
- Tsai EC, Santoreneos S et al. Tumors of the skull base in children: review of tumor types and management strategies. Neurosurg Focus. 2002: 15;12(5).
- Zacharin M. Paediatric management of endocrine complications in McCune-Albright syndrome. J Pediatr Endocrinol Metab. 2005;18:33-41.
- Whitaker SB, Vigneswaran N, Budnick SD, Waldron CA. Giant cell lesions of the jaws: evaluation of nucleolar organizer regions of varying behavior. J Oral Pathol Med 1993; 22(9):402-5.
- Tallan EM, Olsen KD, McCaffrey TV, Unni KK, Lund BA. Advanced giant cell granuloma: a twenty-year study. Otolaryngol Head Neck Surg 1994; 110(4):413-8.
- Carlos R, Sedano HO. Intralesional corticosteroids as an alternative treatment for central giant cell granuloma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93(2):161-6.
- O’Regan EM, Gibb DH, Odell EW. Rapid growth of giant cell granuloma in pregnancy treated with calcitonin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 200; 92(5):532-8.
- Collins A. Experience with anti-angiogenic therapy of giant cell granuloma of the facial bones. Ann R Australas Coll Dent Surg 2000; 15:170-5.