Severe Generalized Gingivitis/Periodontitis and Bleeding
Can you make the correct diagnosis?

This is a 39-year-old white female with a history of mental retardation. She presented in August 2003 to Hospital Dentistry for severe periodontitis, halitosis and loose teeth.
Sorry! you are incorrect
Thrombocytopenia represents a group of disorders with one commonality: a low platelet count. The normal platelet count is 150-400 million cells per milliliter of blood. The average life span of a platelet is 10 days. Platelets are essential for blood to clot; when deficient, bleeding will occur in several forms: in the form of a rash of petechiae or pinpoint red spots, ecchymosis (bruising), and spontaneous bleeding from all orifices including the nose and the oral cavity. Thrombocytopenia develops as a result of either reduced production by the bone marrow or increased breakdown. The latter can happen in the blood vessels (intravascular) or in the liver and spleen (extravascular) (3-4). A number of diseases and medications can cause low production, including inherited diseases, cancer metastasis or primary malignancies of the bone marrow, chemotherapeutic or other drugs, and infections. Patients with thrombocytopenia complain of bruising and bleeding to mild pressure, which happens when the platelet count drops below 80-100 million/ml. Spontaneous bleeding usually occurs when the platelet count drops below 10-15 million/ml. Spontaneous bleeding can start as cutaneous small hemorrhages (purpura) and bleeding from the nose and the oral cavity. Less common are hemorrhage in the gastrointestinal tract, eyes, and in the brain; these all are obviously more serious complications of thrombocytopenia. This disease is first tested by a standard blood count; however, more invasive tests such as bone marrow biopsy may be required for a more specific diagnosis. Bone marrow biopsies are usually handled by hematologists and read by hematopathologists. Treatment of thrombocytopenia depends on the etiology and severity (the presence and absence of bleeding). If induced by drugs, withdrawal of the medications would resolve the disease, spontaneous can resolve without treatment. Other treatment modalities range from the use of steroids, to platelet transfusion, to splenectomy in the worst cases (3-4). The blood workup in this patient was not consistent with thrombocytopenia. Also, besides bleeding, this patient presented with severe periodontitis, ulceration, difficulty moving and non-healing ulcers, all of which are not consistent with thrombocytopenia.
Sorry! you are incorrect
Leukemia is a malignant neoplasm of bone marrow WBC replacing the normal marrow elements. It is clinically classified into acute and chronic types. The acute type is more common in children and is more severe, rapidly growing, and more serious and fatal in comparison to the chronic type, which is more common in adults and can be just as serious as the acute type but may be more responsive to treatment and may go through longer periods of remission. Histologically, it is divided into lymphoblastic/lymphocytic and granulocytic which includes myelogenous and granulocytic types (5-7). A number of factors have been implicated in the etiology of human leukemia such as exposure to radiation, chemicals such as Benzene, and certain viruses. The latter is particularly true with human T-cell lymphotropic virus type 1, which is endemic in Japan. Retroviruses are common in animal leukemia. Chromosomal abnormalities such as Philadelphia chromosome (transition of #22 to #9) are present in over 80% of chronic myelogenous leukemia; similarly, leukemia is up to 15 times more common in patients with certain syndromes such as Down syndrome (trisomy 21) and Klinefelter syndrome. Clinically, patients with leukemia suffer from pancytopenia (anemia, infection and bleeding). Specifically, they complain of fatigue, malaise, headache, lymphadenopathy, bleeding disorders (petechiae, ecchymosis), anorexia, weight loss, and fever. Patients may not manifest many of the aforementioned signs and symptoms until the disease progresses past the early stages. Oral manifestations of leukemia include bleeding, petechiae, ecchymosis, ulcers, and gingival hyperplasia and bone resorption. The gingival swelling is generalized, usually very vascular, and tends to occur more in the interdental papilla area. 90% of patients with acute lymphoblastic leukemia will show oral changes as the disease progresses. The white blood count (WBC) of the acute type may be normal, increased or decreased, and blood film shows immature and atypical white blood cells. Patients may also suffer from prolonged bleeding time. The WBC of the chronic type is increased, sometimes over 500,000/mm3. Leukemia is treated with a variety of approaches including chemotherapy, whole body radiation, and bone marrow transplants. The prognosis depends on the type and stage of the disease. Acute leukemia has a poor prognosis, while chronic has a better prognosis but tends to transform into acute with time (5-7). This patient had gingival changes that could have been described as leukemic gingiva; the skin hemorrhage could also have supported this diagnosis and therefore was seriously considered. However, either the histology nor the blood workup supported a diagnosis of leukemia.
Congratulations! You are correct
The water soluble vitamin C is not produced by humans, but is essential for many important mechanisms in the human body. Deficiency in vitamin C leads to scurvy. Primates and guinea pigs are the only species that cannot produce Vitamin C. It has been known to affect humans since the era of ancient Egypt and was first described as an entity in 1541, when it was believed to be an infectious disease. Vitamin C, or ascorbic acid, is an essential cofactor in a number of cellular activities; the most important is the hydroxylation of collagen fibers, which are the “backbone” of connective tissue, constituting over 60% of bone and dentin. It is present around blood vessels and in and around most organs as the connective tissue that sustains and glues cells together. If collagen fails to hydroxylate, it breaks down, leading to a number of clinical signs and symptoms ranging from leaky blood vessels to brittle bone and dentin. Dr James Lind, an officer in the British Royal Navy, is credited with [1] the discovery of the treatment of scurvy after conducting a study with a group of 12 of his sailors suffering from the disease. He divided them into six pairs, and they all received supplements; two received orange and lemon, two received apple cider, and the other four groups received variations of treatments recommended by the British Royal Navy. The sailors that received citrus fruit recovered quickly, the two that received cider recovered more slowly, and the other four groups showed no improvement. Vitamin C in present in many fruits (not only citrus fruits) and vegetables. Historically, scurvy was found among sailors on long voyages and in times of famine. Today, scurvy is a rare disease in the world and is especially so in the United States. It is known to afflict terminal alcoholics who neglect eating and resort to alcohol for calories. It is also described in infants between the ages of 6 and 24 months, though it is rare before the age of six months; in this case, it is attributed to the consumption of heated cow’s milk and canned food deficient in vitamin C. It is also described in individuals limiting themselves to poor diets that are deficient in Vitamin C, which is the case in this patient. In addition, it is described among those living in poverty and among heavy cigarette smokers, whose vitamin C absorption is lower than normal. Bleeding is the hallmark of the disease, and one of the early signs of scurvy is the development of raised purplish-red spots on the skin, especially perifollicular (around hair follicles) spots on the extremities. These spots represent hemorrhage around hair follicles but can occur anywhere in the body including in the skin, in joints, subperiosteally, within the gingiva, and internally. Oral changes include swollen, red, boggy, hemorrhagic and ulcerative gingiva. Foul breath similar to ANUG is also described. Bone loss and tooth mobility similar to advanced periodontitis are also present. Eating becomes difficult because of the bleeding and pain. Bleeding into muscles, joints and bone is described and is known to be very painful and limiting to motion. Scurvy is successfully treated with vitamin C supplements or food with vitamin C content with excellent results (2).
Treatment
The patient was admitted to the hospital for a full odontectomy with gingival plasty and biopsies of some of the soft tissue (Fig 5). This was done under general anesthesia in the operating room. Laser surgery had to be used to get eschar in order to control hemorrhage. Good hemostasis was achieved by eschar using a CO2 laser. The patient was discharged with both written and oral instructions to her parent regarding nutritional health and was given prenatal vitamins for daily intake. She presented four weeks later with complete clearing of the hemorrhage on the skin (Fig 6) and good healing of the gingival surgery site (Fig 5).
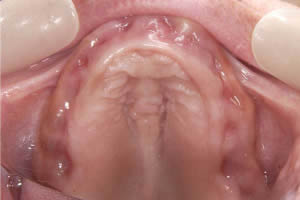
Figure 5. Four weeks post surgery and multivitamin treatment.

Figure 6. Four weeks post multivitamin treatment with no evidence of bleeding. The brown coloration represents hemosiderin aggregates post bleeding. It too would subside.
References
- J. Lind, A treatise of the scurvy. In three parts. Containing an inquiry into the nature, causes and cure, of that disease. Together with a critical and chronological view of what has been published on the subject. , Kincaid and Donaldson, Edinburgh (1753).
- Cheung E, Mutahar R et al. An epidemic of scurvy in Afghanistan: assessment and response. Food Nutr Bull. 2003;24:247-255.
- Finucane D, Fleming P et al. Dentoalveolar trauma in a patient with chronic idiopathic thrombocytopenic purpura: a case report. Pediatr Dent. 2004;26:352-354.
- Wiwanitkit V. Bleeding and other presentations in Thai patients with dengue infection. Clin Appl Thromb Hemost. 2004;10:397-398.
- Wu J, Fantasia JE et al. Oral manifestations of acute myelomonocytic leukemia: a case report and review of the classification of leukemias. J Periodontol. 2002;73:664-668.
- Cooper CL, Loewen R et al. Gingival hyperplasia complicating acute myelomonocytic leukemia. J Can Dent Assoc. 2000;66:78-79.
- Weckx LL, Tabacow LB et al. Oral manifestations of leukemia. Ear Nose Throat J 1990; 69:341-342.