August 2010: Diffuse Radioplaque Expansile Lesion, Right Posterior Maxilla
Can you make the correct diagnosis?
This is a 48-year-old black male who first presented four months ago to his dentist for a routine dental cleaning where swelling of the right posterior maxillary gingiva was noticed.
Sorry! you are incorrect
Given the radiographic findings, the four month history of discomfort and progression of the disease, chronic sclerosing osteomyelitis would be a reasonable condition to include on the differential diagnosis. However, the location is highly unlikely for CSO, the lack of vitality in teeth 1-4 which otherwise look radiographically unremarkable are not supportive of CSO, neither is the histology.
Chronic sclerosing osteomyelitis is a challenging condition to diagnose both clinically and histologically. It has gone through an evolution of names starting with ossifying osteomyelitis used by Thoma in the 1940s and the current name was first used by Shafer in 1957 (1) where he divided it into focal and diffuse. It is described to be by far more common in the mandible, more in females and usually presenting with pain and local swellings with cyclical exacerbations. This is the type of osteomyelitis that most investigators agree that it is not associated with suppuration or fistula formation. Some reports indicate mild suppuration may develop but rarely. It can occur at any age with a wide range including children under the age of ten (1-3). The child type is called “juvenile mandibular chronic osteomyelitis” which affects 6-12 years old children, mostly girls and mainly in the mandible. The adult type is affects 30-40 years of age, twice as common in females but with no race predilection. It is by far more common in the mandible especially posterior mandible (1-3). Patients, children or adults present with a history of years of pain with cyclical exacerbations. Some investigators were successful in isolating E corrodens (2) while most have not been able to grow any micro-organisms. Radiographically: It presents as diffuse, irregular aggregates of bone with indistinct borders. It may mimic Paget’s disease. Histologically, the biopsy shows dense bone with a “mosaic” consistent with a reactive process. The surrounding soft tissue may contain neutrophils during the acute stage and variable number of chronic inflammatory cells, mainly lymphocytes and plasma cells It is indeed a challenge to treat chronic sclerosing osteomyelitis. Antibiotics, especially penicillin and doxycycline and decortications seem to be effective at the early stages and in controlling the disease but resection has occasionally and in rare cases been used (3). Literature indicates that NSAIDS are useful in controlling the intensifying pain. Hyperbaric oxygen is reported to be effective in some cases. If it does not respond to antibiotics or NSAIDS, surgery is indicated (3).
Congratulations! You are correct
The incisional biopsy was read as chondrosarcoma, grade 2 while the surgical specimen revealed a lot more tissue and the diagnosis was changed to chondroblastic osteosarcoma. This is not unusual since the two neoplasms carry many histologic similarities. The age, the location and radiographic changes are supportive of chondrosarcoma.
Chondrosarcoma:
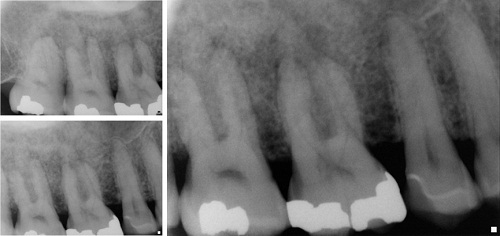
This is a malignant mesenchymal neoplasm of cartilage origin. It is uncommon, especially in the jaws. It occurs more often in the maxilla, particularly in the incisor area. It can occur at any age but is most common in males in the sixth decade of life (7-8). This neoplasm has a low tendency for metastasis. In general, the prognosis is better than that of osteosarcoma, but can vary depending on the stage of the disease. It commonly presents as an asymptomatic swelling with buccal and lingual expansion. Patients may experience unexplained paresthesia, headache, loosening and loss of teeth. Radiographically, it presents as an ill-defined, mottled radiolucency with snowflake or punctate calcifications or diffuse radiopacity (7-8). Sometimes, the teeth will show a widened periodontal ligament space. Histologically, it is characterized by immature and pleomorphic cartilage, but at times the cartilage is benign-looking. It is rare for the cartilage to calcify or differentiate and form bone (7-8). Therapy for chondrosarcoma ranges from wide local excision to radical resection with or without chemotherapy, depending on the stage of disease. The prognosis ranges from good to poor.
Osteosarcoma:
Osteosarcoma is the most common, non-hematopoietic, primary malignancy of bone. It is a malignancy of mesenchymal cells that have the ability to produce osteoid or immature bone. Osteosarcoma of the jaw represents 6-9% of all osteosarcomas. Paget’s disease and prior radiation therapy are associated with an increased risk of developing osteosarcoma. The mean age for patients with gnathic osteosarcomas is about 33 years, which is 10-15 years older than the mean age of osteosarcomas of the long bones (9-11). The maxilla and mandible are involved with equal frequency. Patients with osteosarcoma may experience pain, swelling, paresthesia and/or loosening of teeth (9-11). These tumors may vary greatly in radiographic presentation. Some lesions display an entirely radiolucent process, while others may demonstrate dense sclerosis in the affected area as is the case in this patient. However, the majority of osteosarcoma cases present as a mixed radiolucent and radiopaque lesions. Other radiographic findings include: symmetric widening of the periodontal ligament space (PDL), diffuse borders of the lesion, periosteal reaction, “spiked” roots or the classic “sunburst” or “sun ray” appearance caused by osteophytic bone deposition at the periphery (9-11). These changes may be evident on CT, periapical, panoramic, and/or occlusal radiographic studies.
In addition to the wide range of possible radiographic presentations, the histologic findings of osteosarcoma also display a considerable amount of variability. The vast majority of conventional osteosarcomas are classified as osteoblastic, chondroblastic, or fibroblastic. The division of the specific histologic type is based on the predominant histologic pattern of the tumor. To make a diagnosis of osteosarcoma, the direct production of osteoid by malignant mesenchymal cells must be present. In addition to osteoid, the tumor cells may produce cartilaginous matrix (chondroblastic osteosarcoma) or a high-grade spindle cell stroma (fibroblastic osteosarcoma). If the majority of the tumor is composed of an osteoid product, then it is classified as osteoblastic osteosarcoma. Chondroblastic osteosarcoma is the most common histologic type seen in the jaws. The grading of osteosarcoma is based on the amount of cellular atypia; they typically graded on a scale of 1 to 4, with 4 being the highest grade (9-11).
Osteosarcoma is a persistent malignancy. Its most important prognostic indicator is the ability to obtain initial complete surgical removal. Untreated, conventional osteosarcoma is universally fatal. Osteosarcoma has an aggressive local growth potential and a propensity to spread systemically via hematogenous routes. The lung is the most frequent site of metastasis. Metastases from mandibular lesions are more frequent than from maxillary lesions. Today, therapy is typically multi-disciplinary, focusing on both local and systemic manifestations of osteosarcoma, thus incorporating surgery and chemotherapy (9-11). The use of this combined approach has resulted in a survival rate of 60-80%. In a 1997 study performed at the University of Washington, patients diagnosed with head and neck osteosarcoma had an overall 5-year survival rate of 72% (10).
References
- WG Shafer, Chronic sclerosing osteomyelitis, Oral Surg. 1957:15; 138-142.
- Marx RE, Carlson ER, Smith BR, Toraya N. Isolation of Actinomyces species and Eikenella corrodens from patients with chronic diffuse sclerosing osteomyelitis. J Oral Maxillofac Surg. 1994;52(1):26-34.
- Y. Suei, K. Tanimoto, M. Miyauchi and T. Ishikawa, Partial resection of the mandible for the treatment of diffuse sclerosing osteomyelitis: Report of four cases, J Oral Maxillofac Surg. 1997: 55; 410
- MacDonald-Jankowski DS. Fibro-osseous lesions of the face and jaws. Clin Radiol. 2004;59:11-25
- Rao VV, Schnittger S et al. G protein Gs alpha (GNAS 1), the probable candidate gene for Albright hereditary osteodystrophy, is assigned to human chromosome 20q12-q13.2. Genomics. 1991;10:257-261
- Neville BW, Damm DD, Allen CM, Bouquot JE. Oral & Maxillofacial Pathology. 3rd ed. Philadelphia: WB Saunders Company 2009.
- Anil S, Beena VT et al. Chondrosarcoma of the maxilla. Case report. Aust Dent J. 1998;43:172-174.
- Hayt MW, Becker L et al. Chondrosarcoma of the maxilla: panoramic radiographic and computed tomographic with multiplanar reconstruction findings. Dentomaxillofac Radiol. 1998;27:113-116.
- Bennett JH, Thomas G et al. Osteosarcoma of the jaws: a 30-year retrospective review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:323-332
- Oda D, Bavisotto LM et al. Head and neck osteosarcoma at the University of Washington. Head Neck 1997;19:513-523.
- Slootweg PJ, Muller H. Osteosarcoma of the jaw bones. Analysis of 18 cases. J Maxillofac Surg 1985;13:158-166.
Sorry! you are incorrect
The cotton wool/ground glass appearance of the periapical radiograph should make one think of fibrous dysplasia and so does the location. However, the age of the patient, the persistent four month discomfort and lack of vitality in teeth #s 1-4, are not supportive of the clinical behavior of FD, neither is the histology.
Fibrous dysplasia is a tumor-like developmental and hamartomatous disorder of bone that presents in three forms: monostotic, polyostotic and craniofacial. It is common, affecting 7% of all benign bone tumors. The monostotic form constitutes approximately 80% of all fibrous dysplasia cases. It affects males and females equally, occurs in childhood and adolescence and usually completes growth by the age of 30. The craniofacial form affects the maxilla and the craniofacial complex, and is more aggressive than the monostotic form. Polyostotic cases constitute 10% of all FDs; they may (such as McCune-Albright) or may not (Jaffe) be associated with multiple endocrine disorders (4, 6). The etiology of FD is not clear but a mutation (GNAS 1) has been identified at multiple chromosomes. This gene can occur at all ages, even in infancy (5). Some of the FD cases are clinically asymptomatic and are found incidentally; many present with swelling and deformity, and rare cases involve pain. Swelling of the maxilla or mandible is the most common presentation. It may involve bones other than the maxilla, including the zygoma, sphenoid and frontal. Monostotic FD is usually unilateral and is known to displace the surrounding teeth, but is otherwise firmly seated. It is usually slow-growing, but rapid growth has been described, especially during puberty. With rapid growth, temporary pain is also described. The radiographic appearance, especially of the maxilla, is classically described as a ground glass appearance where fine radiopacity is noted (4-6). The mandibular lesions are much more deceiving; more variability exists, thus making the radiographic diagnosis more difficult. It ranges from cystic radiolucency to a classical ground glass radio-opacity. Histologically, it consists of vascular fibrous connective tissue stroma with irregular (Chinese character) spicules of woven bone. Giant cells may be seen. At times, artifactual shrinkage of the connective tissue from bone is noted. Many cases do not need treatment; those that do are best treated with surgical recontouring of the affected bone to address aesthetic or functional concerns (4-6). This is preferably performed after cessation of growth due to the high incidence of requirement for secondary procedures. Some sources report a tendency for increased growth of the lesion following surgical intervention, but the evidence for this is weak. Even if recontouring is performed in adulthood, multiple procedures are frequently required. This may be due to inadequate removal, continued growth or the ossification of the subperiosteal hematoma, which is difficult to avoid due to the very vascular nature of the dysplastic bone. Radical excision with primary reconstruction of the affected bone has been suggested, but is not widely accepted. Radiation therapy has been used in the past and is successful in stopping growth of the lesion. Unfortunately, a significant incidence of development of osteosarcoma in the irradiated bone prohibits the use of this modality. Treatment with bisphosphonates has also been successfully used. The overall prognosis is good with proper clinical management.