An Ulceration of the Tongue
Can you make the correct diagnosis?
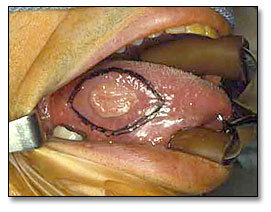
The clinical examination revealed a 3×5 cm ulcerated white mass on the right mid-lateral border of the tongue of a male patient.
Sorry, this is not the correct diagnosis.
The oral cavity is frequently afflicted with surface ulcerations: single and multiple, superficial and deep, acute and chronic, of local and of systemic origin. For that reason, it is very important that clinicians view oral ulceration with some attention to etiology.
It is important to state that most single oral ulcers are trauma induced and can occur at any age. The source of trauma can be a sharp tooth, an ill-fitting denture or a sharp denture edge, a broken filling, a bite, or any other similar irritant. Chronic single ulcers, especially those associated with dentures, may have rolled borders because of scarring occurring during the healing process. The rolled border-type ulcers are frequently mistaken for SCC. Elimination of the source of trauma will help healing of the ulcer within two to three weeks.
Sometimes, however, the source of trauma is difficult to identify, and even when identified and removed, the ulcers do not heal and may remain persistent for months. A biopsy of a non-healing ulcer is warranted for two reasons: to rule out malignancy, such as squamous cell carcinoma, and to initiate healing. This is especially true with ulcers on the lateral border of the tongue, which happens to be a common location for traumatic ulcers. It is good practice to refer patients with ulcers of the mouth when they fail to heal within 2-3 weeks.9 The location in is this case (Figure 1) is consistent with traumatic ulcer, but the histology is not supportive of that diagnosis.
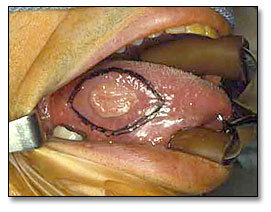
Figure 1. This clinical photograph represents the lesion before surgery. White, non-healing rolled-bordered ulcer on the mid lateral border of Tongue.
Sorry, this is not the correct diagnosis.
These ulcers are also known by other names, including eosinophilic ulcer, eosinophilic granuloma of the tongue (which is not related to eosinophilic granuloma of the bone as in histiocytosis X disease), and traumatic ulcerative granuloma with stromal eosinophilia (TUGSE). Traumatic granuloma commonly occurs on the dorsal and lateral tongue in patients with a history of trauma. It may affect patients of all ages, including infants (Riga-Fede disease occurs during the first year of life as a result of chronic trauma in the sublingual area to the baby lower incisors during breastfeeding). Traumatic granuloma tends to occur more in males than females. Histologically, these ulcers are deep lesions involving the underlying muscle, which may explain the process of slow healing and the tissue eosinophilia. Healing may take up to eight weeks. Eosinophils are found in areas of muscle damage. Clinically, traumatic granulomas tend to be deep ulcers with rolled borders mistaken for SCC.10 Like traumatic ulcer, the location is consistent with traumatic granuloma while the histology is not supportive of it.
No content for this section. Make sure you wrap your content like this:
Content here
Congratulations. You are Correct!
No content for this section. Make sure you wrap your content like this:
Content here
Oral squamous cell carcinoma is a highly aggressive neoplasm that currently ranks as the fifth most common malignant neoplasm worldwide and accounts for an estimated 90% of oral malignancies.1 The incidence of oral SCC is incessantly increasing.
Oral squamous cell carcinoma (OSCC) is annually diagnosed in over 30,000 people in the United States and over 570,000 worldwide.1, 2 The five-year survival rate lies between 35% and 50%.3 Despite sophisticated developments in cancer diagnosis and treatment throughout the last 20 years, this rate has disappointingly only slightly improved since the 1950s.2 High mortality persists, and over 8000 people die of oral cancer each year in the United States alone.3
Oral SCC occurs predominantly in males over the age of 40 years, with an observed male to female ratio of 2:1 generally and 1.4:1 in the USA.1 Excluding the outer lip, the most common sites (in decreasing order) are ventral and lateral surfaces of tongue (25-50%), floor of mouth (15%), gingiva (12%) and palate (9%). The buccal mucosa and retromolar pad areas (3%) have a relatively low incidence of occurrence3 unless the patient is a chronic smokeless tobacco user. Oral SCC varies in presentation from deceptively innocent-looking to obviously malignant. It may present as a non-healing ulcer, or as red, white or mixed red-and-white lesions. Characteristic signs of oral SCC are non-healing ulcer, ulcer with rolled borders, fungation, fixation and induration. Rarely, OSCC may present as unexplained, asymptomatic lateral neck lymphadenopathy. 1, 2, 3 The location, age, risk factors and clinical presentation of this case are typical of OSCC.
Tongue SCC is the most common type; it is usually found on the lateral and ventral surfaces. The dorsal surface of tongue is rarely involved. If it occurs, it is usually in patients with a history of syphilitic glossitis, a condition that is extremely rare today.1, 2 Squamous cell carcinoma of the posterior tongue is more aggressive than that of the anterior. 78% of base of tongue carcinomas show early metastasis, especially to regional lymph nodes. 69% of tongue carcinomas show evidence of metastasis at admission. Oral SCC is most commonly associated with chemically induced mutagenesis, specifically tobacco and alcohol use.4
Tobacco use is described in over 75% of oral SCC patients.1, 4 Tobacco and alcohol have been shown to act synergistically in the development of OSCC 5. Human papilloma virus (HPV) has also been found to have a high prevalence in oral cancer, especially in younger patients with no history of tobacco use.5 Other factors include poor oral hygiene, syphilis, chronic candidiasis, iron and dietary deficiencies, herpes simplex and various other immunologic factors5, and lichen planus—especially the persistent erosive lichen planus.6
Determination of the prognosis of OSCC is based on the clinical stage and histological classification. Although OSCC is a diagnosis made by histology, surgeons tend to depend exclusively on the TNM classification system for clinical staging and treatment decisions.7 Oral SCC is graded according to the degree of the neoplastic epithelial cell differentiation as described by Broders8, suggesting that the more differentiated the histology, the better the prognosis. This is not actually the case clinically, since prognosis is more dependent on the TNM staging system. Histological grading ranges from well to moderately to poorly differentiated. The histology of this case was within the moderately well differentiated range.
In general, the more posterior the OSCC, the worse the prognosis. The most important prognostic sign is the presence or absence of metastases at the time of diagnosis. The prognosis thus improves when the lesion is detected early. Oral SCC patients die mainly of infection due to lowered resistance or of hemorrhage if the tumor erodes through one of the main blood vessels.
No content for this section. Make sure you wrap your content like this:
Content here
Treatment consisted of right hemiglossectomy, right selective neck dissection, levels I-V and radial forearm free flap reconstruction (Figure 2). Due to the size of the tumor and its close proximity to the surgical margins, post-operative radiation therapy was recommended. The patient received 6750 cGY of radiation and recovered well, as illustrated in Figure 3 (three years’ postoperative follow-up).

Figure 2. This photograph is taken soon after surgery demonstrating the hemiglossectomy procedure with a forearm free flap reconstruction.

Figure 3. Post operative photograph demonstrating full healing of the area grafted with intact forearm free flap.
No content for this section. Make sure you wrap your content like this:
Content here
- Food, Nutrition, and the Prevention of Cancer: a global perspective. World Health Organization 1997.
- Examinations for oral cancer – United States. MMWR. Morb.MortalWkly Rep. 43:198 (1992).
- Bundgaard T, S Bentzen, et al. Histopathologic, stereologic, Epidemiologic, and clinical parameters in the prognostic evaluation of squamous cell carcinoma of the oral cavity. Head & Neck. 18:142-152 (1996).
- Barasch A, DE Morse, et al. Smoking, gender, and age as risk factors for site-specific intraoral squamous cell carcinoma. Cancer 73:509-513 (1994).
- Syrjanen SM, KJ Syrjanen et al. Human papillomavirus (HPV) DNA sequences in oral precancerous lesions and squamous cell carcinoma demonstrated by in situ hybridization. J Oral Pathol. 17:273 (1988).
- Holmstrup P, JJ Thorn, et al. Malignant development of lichen planus-affected oral mucosa. J Oral Pathol. 17:219-25 (1988).
- American Joint Committee for Cancer Staging and End Result Reporting. (1983).
- Broders AC. Squamous-cell epithelioma of the lip: a study of five hundred and thirty-seven cases. JAMA. 74(10):656-64 (1920).
- Houston, G. traumatic ulcers. E-Medicine.com, updated July 02
- Alawi, F. Eosinophilic Ulcer. E-Medicine.com. Updated May 02
- Shah A, E-Medicine.com. Updated July 03
Sorry, this is not the correct diagnosis.
The oral cavity is a site where a number of acute and chronic infectious diseases occur as a local disease or as a manifestation of a systemic disease. They include diseases of viral, fungal and bacterial origin. They usually present in multiple or in a diffuse manner ranging from ulcers to small and nodular lesions to verrucoid lesions. Rarely would infectious diseases present as a single ulcer with rolled border, simulating an OSCC. Those include ulceration induced by mycobacterium tuberculosis, deep fungal infection such as blastomycosis and histoplasmosis and chancre of primary syphilis. Oral manifestations of tuberculosis and histoplasmosis are unusual without lung involvement and a disseminated disease and occur more in immune compromised patients. Gingiva and the mandibular vestibule are more common locations but tongue can occasionally be affected. Chancre can occur in any location, including the tongue, lips and hard palate. As mentioned previously, single oral ulcers of infectious disease origin are a rare occurrence and should be kept low on the differential diagnosis list.11 The histology in this case was not supportive of an infectious process.