Return to Case of the Month Archives
Fosamax induced osteonecrosis
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Contributed by
Dr. Jose Bagan
Valencia University, Valencia, Spain
Case Summary and Diagnostic Information
This is an 82-year-old white female from Spain diagnosed with osteoporosis a few years prior. She was treated with Fosamax at a dosage of 70 mg per week for three years.
Diagnostic Information Available
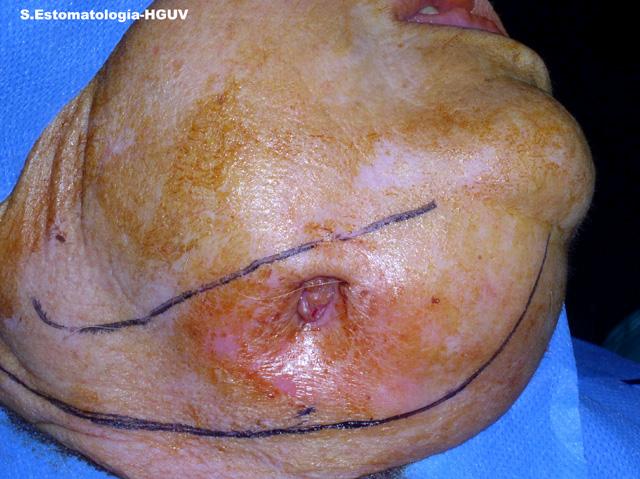
This is an 82-year-old white female from Spain diagnosed with osteoporosis a few years prior. She was treated with Fosamax at a dosage of 70 mg per week for three years. The patient presented to the Department of Oral Medicine at Valencia University complaining of pain in the right posterior mandible. Upon examination, the right posterior mandibular alveolar ridge was found to be covered with intact mucosa except for a small ulcer with a small fistula. The skin overlying that area, however, showed evidence of a cutaneous fistula (Fig 1) oozing pus and blood. A panoramic radiograph confirmed that the origin of the cutaneous fistula was in the posterior mandible (Fig 2). The patient’s past medical history is significant for arthritis and osteoporosis.
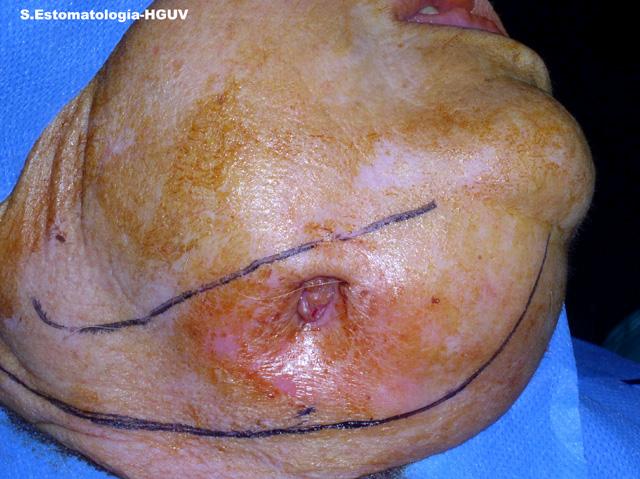
Figure 1. This is a clinical view of the lesion after six months of conventional treatment. The submandibular skin shows a cutaneous fistula.

Figure 2. This is a panoramic radiograph demonstrating a large and ill-defined radiolucent radiopaque lesion in the right posterior mandible with a pathologic fracture and bony sequestration.
Her past medical history is significant for Arthritis and osteoporosis.
Clinically the oral mucosa covering the alveolar ridge was mostly intact and unaffected except for a small ulcer with a small fistula. The skin covering the mandible, however, showed a large fistula which oozed pus for a period of 6 months. Radiographic findings were significant for large pieces of bony sequestra in the posterior mandible surrounded by irregular radiolucency, with a mandibular fracture (Fig 2). The patient experienced pain that required many analgesic drugs. The CT-scan supported the radiographic findings of the panoramic view.

Figure 2. This is a panoramic radiograph demonstrating a large and ill-defined radiolucent radiopaque lesion in the right posterior mandible with a pathologic fracture and bony sequestration.
Histologic examination revealed multiple pieces of decalcified hard and soft tissue. The latter comprised a significant portion of the specimen and was mostly granulation tissue covered by stratified squamous epithelium and infiltrated by many neutrophils, plasma cells and lymphocytes (Fig 4). The bony fragments were mostly lamellar in type with Haversian systems devoid of viable osteocytes. The bony fragments show evidence of external resorption covered by bacterial colonies of mixed oral flora (Fig 5).
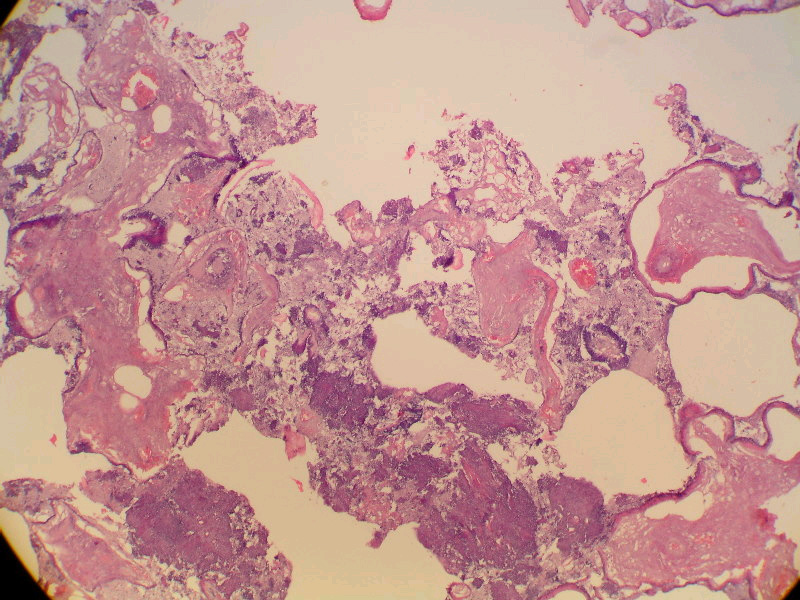
Figure 4. Low power (x100) histology illustrates bony trabeculae surrounded by loose and vascular granulation tissue with many inflammatory cells.
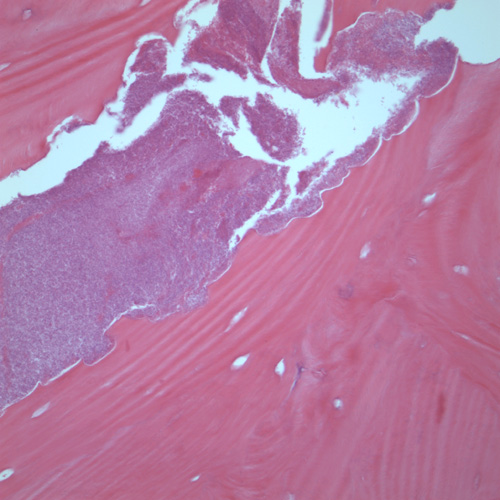
Figure 5. Higher power (x200) histology illustrates bony trabeculae devoid of viable osteocytes. The bone shows evidence resorption surrounded by bacterial colonies.
After you have finished reviewing the available diagnostic information