Return to Case of the Month Archives
Unilocular radiolucency around impacted tooth #32
Dolphine Oda, BDS, MSc
doda@u.washington.edu
Contributed by
Dr. Creed Haymond & Glenn Taylor
Oral Surgery and General Dentistry, Utah
Case Summary and Diagnostic Information
This is an 18-year-old Caucasian female who was referred by her general dentist to an oral surgeon for the removal of four third molar teeth and the evaluation and management of a unilocular radiolucent lesion associated with impacted tooth #32. The radiolucency was corticated and was displacing tooth #32 inferiorly. There was no evidence of facial swelling or pain.
Diagnostic Information Available
This is an 18-year-old Caucasian female who was referred by her general dentist to an oral surgeon for the removal of four third molar teeth and the evaluation and management of a unilocular radiolucent lesion associated with impacted tooth #32. The radiolucency was corticated and was displacing tooth #32 inferiorly. There was no evidence of facial swelling or pain.
The patient has no history of tobacco and alcohol use and is otherwise in good health. The patient is not on any medications and has no known allergies.
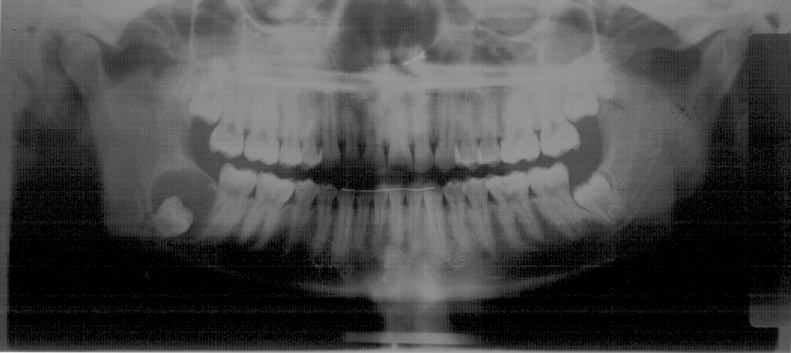
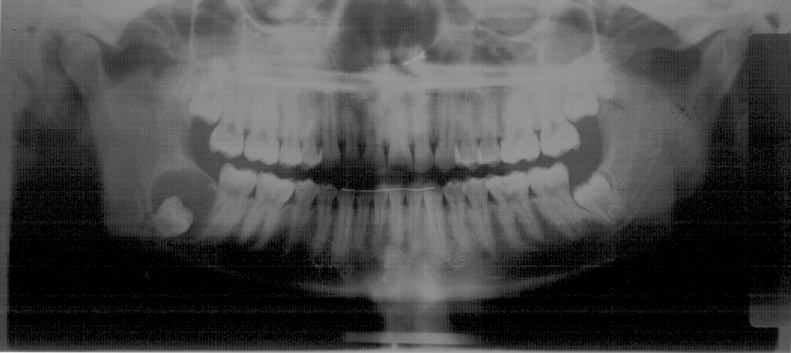
This patient was referred to the oral surgeon (CH) for third molar removal as well as the removal and evaluation of a large cystic lesion around tooth #32 (Fig 1). The patient has all four of her third molars; three (teeth #s 1, 16 and 17) are close to eruption and the fourth (#32) is impacted. Tooth # 32 shows a large, unilocular radiolucency with smooth and corticated borders displacing the tooth inferiorly, leaving the jaw bone thin and vulnerable. The radiolucency surrounds the crown of tooth # 32 from the cemento-enamel-junction (CEJ) to CEJ. Despite the size of this lesion, there was no clinical evidence of significant expansion.
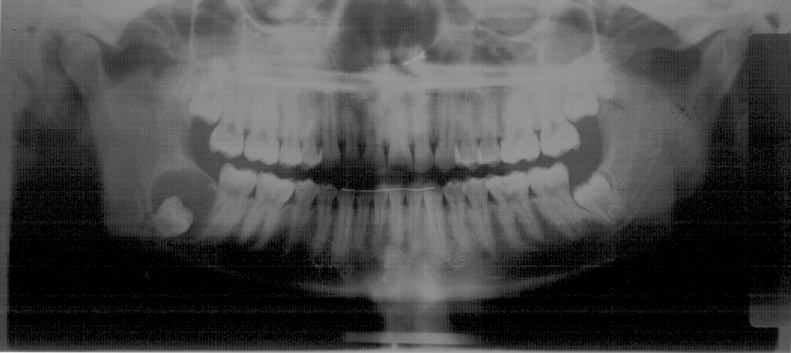
Figure 1. This is a panoramic view taken at the first clinical presentation Dec 2005. The radiograph demonstrates a corticated unilocular radiolucency around impacted tooth #32 with the tooth displaced inferiorly.
Figure 2. Kaposi’s sarcomas involving the soft palate and anterior hard palate. Note the purplish-red color, both are exophytic and the soft palate lesion is obstructive to the oropharynx.
Histologic examination revealed an odontogenic cystic structure and a benign neoplasm of odontogenic epithelial origin. The latter is either associated with or arising from the odontogenic cyst. This neoplasm is also cystic and is made up of neoplastic lining epithelium, epithelial islands within the superficial connective tissue and a fibrous connective tissue wall. The lining epithelium shows changes within the basal and parabasal cell layers consistent with those of an ameloblastoma. The basal cell layer is columnar and palisaded with polarized nuclei (Figs 3 & 4) with multiple layers of spindle shaped epithelial cells. In focal areas, epithelial islands with palisaded and polarized periphery and stellate reticulum cells in the center are noted in close proximity of the lining epithelium (Fig 5). Also, in focal areas, a true cystic structure with non-keratinized stratified squamous epithelium consistent with a dentigerous cyst is identified.
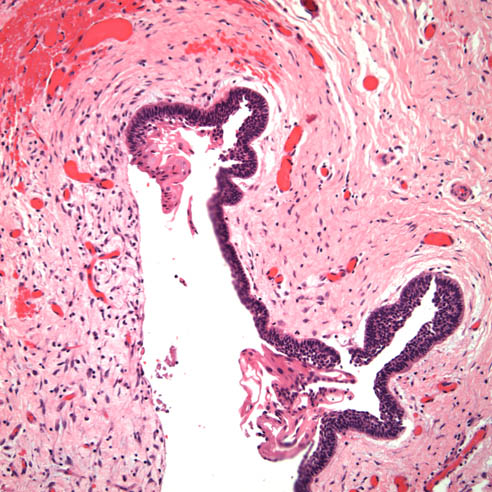
Figure 3. Low power (x40) histology shows a benign cystic neoplasm of odontogenic epithelial origin. Note the palisaded columnar epithelial cells with dark nuclei present at the basal cell layer. These changes are consistent with early neoplastic changes.
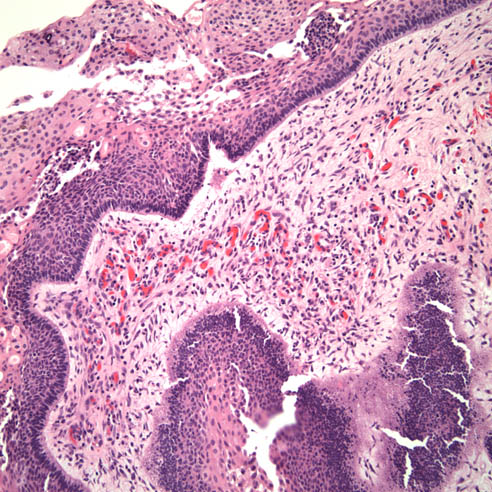
Figure 5. Higher power (200) histology shows the cystic neoplasm with epithelial islands in the superficial connective tissue wall. The epithelial islands have palisaded and polarized borders with reversed polarization and a center filled with stellate reticulum.
After you have finished reviewing the available diagnostic information