Left Facial Swelling with Mild Fever
Can you make the correct diagnosis?

This is a 16-year old white male referred by the orthodontist to the Oral Surgeon to evaluate a single radiolucent lesion in the anterior mandible. It was discovered during routine radiographic evaluation by his orthodontist. The lesion was asymptomatic; there was no swelling or pain.
Sorry! you are incorrect
The Periapical cyst is also known as radicular cyst and apical periodontal cyst, among several other names. It is the most common odontogenic cyst and is inflammatory in nature (1). It is capable of destroying bone, displacing teeth, expanding jawbone, and at times causing tooth mobility depending on the size of the cyst. About 75% of these cysts occur in the maxilla associated with the central incisors and 25% in the mandible associated with the molar teeth. They are more common in males. The associated teeth are non-vital and are usually not painful unless are infected. Radiographically, evidence of loss of the lamina dura and widening of the apical periodontal ligament are present. Histologically, it is made up of a cystic cavity lined by epithelium, which in turn is supported by granulation tissue. The lumen may be filled with necrotic and cellular debris, cholesterol cleft, extravasated erythrocytes or a combination of any of these. It can also be empty depending on the content of the lumen, fluid, or semisolid material. The teeth associated with this lesion were vital and the lamina dura and periodontal ligament showed no evidence of any changes. The histology was not supportive of a periapical cyst (1).
A corticated and unilocular radiolucency in the jaws should be considered to be a cyst first and foremost. Conditions such as benign fibro-osseous lesion, traumatic bone cavity and salivary gland depression can also share similar radiographic features. These lesions, however, are not as common as the odontogenic cysts.
Sorry! you are incorrect
The Odontogenic keratocyst (OKC) is an aggressive odontogenic cyst, known for its rapid growth ad its tendency to invade the adjacent tissues, including bone. It has a high recurrence rate and is associated with basal cell nevus syndrome. It affects patients in the age ranges of 20-29 and 40-59, but cases in patients ranging in age from 5 to 80 years have been reported (2). The distribution between sexes varies from equal distribution to a male-to-female ratio of 1.6:1, except in children. Odontogenic keratocysts may occur in any part of the upper and lower jaw, with the majority (almost 70%) occurring in the mandible. They occur most commonly in the angle of the mandible and ramus (3). Radiographically, OKCs present predominantly as unilocular radiolucencies with well-defined or sclerotic borders; they may also present as multilocular radiolucencies, but rarely. OKCs commonly present as unilocular radiolucency with scalloped borders. Teeth associated with OKC are vital. OKCs grow to sizes larger than any other odontogenic cysts. They usually penetrate the bone rather than expand it and grow in an anterior to posterior direction (2, 3). Despite this aggressive growth, they often remain asymptomatic, thus growing to large sizes and hollowing the bone. For more details on OKC, please review the March 2004 Case of the Month. The vital teeth and radiographic findings in this case are strongly supportive of OKC; however, the histology and the clinical finding of an empty cavity would not be consistent with OKC.
Sorry! you are incorrect
Focal cemento-osseous dysplasia is a reactive lesion, similar to periapical and florid cemento-osseous dysplasia, except that it presents as a single lesion in the posterior mandible. Radiographically, it goes through all three radiographic stages—completely radiolucent to mixed to predominantly radiopaque with radiolucent rim—similar to those of central ossifying fibroma (5, 6). The associated teeth are vital. It presents mostly in white females around 38 years of age. The age of the patient, the location, and the histology are not supportive of traumatic bone cavity.
Sorry! you are incorrect
Central ossifying fibroma is a benign neoplasm of bone origin that presents as a well-demarcated to corticated complete radiolucency to a mixed radiolucent/radiopaque mass with a peripheral radiolucent rim (4, 5). It is a slow-growing, expansile lesion with characteristic downward expansion of the inferior border of the mandible. It can also expand buccally and lingually. The associated teeth are vital. It is common in young adults around 35 years of age and is five times more likely to occur in females than males. It affects the posterior mandible in about 90% of cases. The age of the patient, the location and the histology are not supportive of traumatic bone cavity.
Congratulations! You are correct
The jawbones are subject to many cysts, mostly odontogenic (of tooth) origin, some developmental (of non-tooth origin), while others are cyst-like or pseudocyst structures such as the salivary gland depression and traumatic bone cavity. Traumatic bone cyst is best called traumatic bone cavity since this condition does not represent a true cyst. Traumatic bone cavity is not unique to the jawbones; it is also described in the long bones and is known as a simple solitary bone cyst occurring mostly in the humerus or femur, close to the epiphyseal plate (9). The long bone simple cyst is similar to the jaw traumatic bone cavity radiographically and occurs in the same age range. Trauma has been suggested as the etiology along with other non-substantiated theories such as cystic degeneration of a preexisting tumor or of the fatty marrow in the area.
Some reports suggest that it is more common in males (10) while others report equal distribution between males and females (9). The long bone counterpart is more common in males by a ratio of 2.5:1. Most reports agree that the average age of occurrence is below 20 years of age (9, 10). These lesions can occur, but are uncommon, over the age of 30. Kaugars reported a higher number of traumatic bone cavity in African American females compared to the literature (9). They were over the age of 30 (9). This may suggest an association with florid cemento-osseous dysplasia. The mandible is the most commonly affected area, where over 95% of the cases occur, especially in the posterior premolar-molar area. They rarely extend to the ramus and are known to cross the midline anteriorly. In one study, 27% were anterior to the canine and some crossed the midline. They are usually unilocular and radiolucent, typically above the alveolar canal and in many cases with a scalloped superior border spreading between the roots of teeth. The latter are vital and are frequently found hanging within the empty cavity. About 25% of the lesions present in the anterior mandible apical to the canine tooth and usually are round and unilocular, which can be mistaken for a periapical lesion leading to an unnecessary endodontic treatment. Therefore, it is important to test the vitality of the teeth and carefully examine the radiographs for changes consistent with a periapical granuloma or cyst. Large, expansile and multilocular traumatic bone cavities have been described, but are very rare. The margins of these lesions range from very well defined to corticated to punched out radiolucency. The majority of lesions are asymptomatic; Kaugars et al reported 26% of their cases were symptomatic and were expansile. Pathologic fractures associated with traumatic bone cavity have been described in the jaws, but are rare. They are however more common with those of the long bones.
Clinically, surgeons almost always report an empty cavity at entrance; occasionally straw-colored fluid is described to be present. Blood clot is also present occasionally. The bony cavity is scraped to generate bleeding, which is considered the treatment of choice for this condition. Other methods of treatment have been tried, such as packing the curetted cavity with autogenous blood, autogenous bone and hydroxyapatite (10). Various other reports demonstrate healing of traumatic bone cavity after injection of autogenous blood, after aspiration and after endodontic treatment. These lesions may spontaneously heal, but rarely. Biopsy material consists of fragments of viable bone and loose connective tissue, as reported in our case. Osteoclast-like giant cells have also been described in a few cases (9). Exploration surgery usually leads to healing. Recurrence is rare.
Treatment
Vestibular incision was performed under general and local anesthesia. A window through the buccal cortex was opened to a completely empty cavity. There was no evidence of fluid, lining epithelium or semisolid material. The bony cavity was curetted to generate bleeding. The area was sutured. Teeth #s 1 and 16 were also removed. Patient was placed on 500mg of amoxicillin three times per day for 10 days. Postoperative healing was uneventful. Sutures were removed seven days after surgery. Four weeks’ postoperative healing is demonstrated in Figure 2.
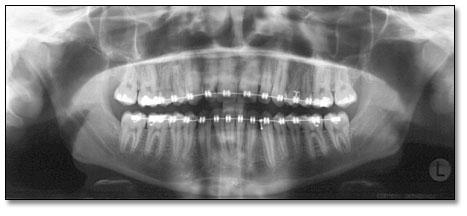
Figure 2. Four-week post surgical panoramic view demonstrating a smaller unilocular radiolucency with cloudy consistency—consistent with early calcification. Teeth #s 1 and 16 are extracted.
References
- Delbem AC, Cunha RF et al. Conservative treatment of a radicular cyst in a 5-year-old child: a case report. Int J Paediatric Dent. 2003. 13: 447-450.
- Shear M. Odontogenic keratocysts: natural history and immunohistochemistry. Oral Maxillofacial Surg Clin N Am. 2003; 15: 347-362.
- Oda D, Rivera V et al. Odontogenic keratocyst: the northwestern USA experience. J Contemp Dent Pract. 2000 Feb 15; 1(2): 60-74.
- Su L, Weathers DR, et al. Distinguishing features of focal cemento-osseous dysplasias and cemento-ossifying fibromas: I. A pathologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997 Sep; 84(3): 301-9.
- Su L, Weathers DR, et al. Distinguishing features of focal cemento-osseous dysplasia and cemento-ossifying fibromas: II. A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997 Nov; 84(5): 540-9
- MacDonald-Janowski DS. Florid cemento-osseous dysplasia: a systematic review. Dentomaxillofacial Radiology 2003; 32: 141-9.
- Phillips A, Yates C. Case report: anterior lingual mandibular cortical bone concavity. Dental Updates. 2004; 31: 175-176.
- Bsoul SA, Tereshalmy GT et al. Developmental submandibular salivary gland depression. Quintessence Int. 2002; 33: 242-243.
- Kaugars GE, Cale AE. Traumatic bone cyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1987; 63: 318-324.
- Dellinger TM, Holder R et al. Alternative treatments for a traumatic bone cyst: a longitudinal case report. Quintessence Int. 1998; 29: 497-502.
Sorry! you are incorrect
Salivary Gland Depression (Static Bone Cyst) is a developmental defect believed to be a defect or depression caused by pressure from growing salivary gland tissue. The most common is the submandibular gland depression located in the lingual aspect of the mandible below the second molar tooth; the second most common type of depression is caused by the sublingual gland present in the lingual mandible below or around the canine tooth. The least common type is the parotid gland depression in the upper and lingual ramus. This condition is usually asymptomatic and tends to occur more often in males. They present as small and round to large and ovoid, usually well-defined radiolucencies (7, 8). The submandibular depression is usually below the mandibular canal (8). This is true of the posterior mandible, but not of the sublingual gland defect in the anterior mandible. Occasionally, they can be bilateral; this is especially true of the posterior mandible. If biopsied, they usually yield normal salivary gland tissue and occasionally fatty tissue and muscle. No treatment is necessary for these lesions. The submandibular depression is the most radiographically diagnostic and the sublingual is the least diagnostic because of its inconsistent radiographic presentation and for that reason, surgical exploration is indicated to rule out other lesions (7). The radiographic presentation of this case is consistent with that of sublingual salivary gland depression. The histology, however, is not.