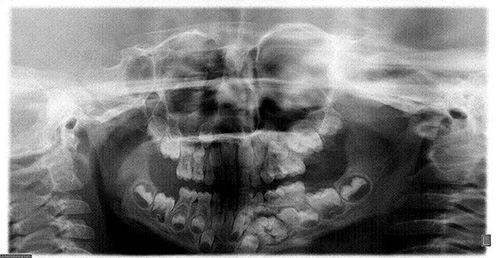
Mixed radiolucent radiopaque lesion
Can you make the correct diagnosis?
This is a 5-year-old white male who presents with a large radiolucent and radiopaque lesion associated with an impacted tooth #22.
Congratulations! You are correct
Whether complex or compound, hamartoma or neoplasm, odontoma is the most common odontogenic tumor, accounting for 22% of all odontogenic tumors. It is of mixed epithelial and mesenchymal origins. It is usually associated with unerupted teeth. It can occur at any age, but is most common in the first two decades of life, with an average age of 14 or 18. It is slightly more common in females and more common in the maxilla, especially the anterior maxilla, than in the mandible. Compound odontomas are more common in the anterior jaws, while complex odontomas occur more often in the posterior jaws. In about 80% of cases, they are associated with impacted or unerupted teeth. Radiographically, odontomas present as a well-circumscribed radiolucency resembling a dental follicle or dentigerous cyst with one or multiple radiopaque pieces resembling teeth. Compound odontomas tend to occur between teeth and tend to be composed of multiple small tooth-like structures, while complex odontomas tend to occur in the posterior jaws and present as a conglomerate mass. Both types are made up of enamel matrix, dentin, cementum, and dental pulp surrounded by a dental follicle or cyst. Histologically, the tooth-like structures are arranged in a uniform manner similar to the normal tooth. The structures in complex odontomas are mixed and disorganized. These lesions are benign and are conservatively treated with simple curettage. Recurrence is not described; if it recurs, one must rule out other odontogenic lesions such as calcifying odontogenic cyst and ameloblastic fibro-odontoma.
References
- Vengal M, Arora H, Ghosh S. Large erupting complex odontoma: a case report. J Can Dent Assoc. 2007 Mar;73(2):169-73.
- Noonan VL, Gallagher G, Kabani S. Compound and complex odontomas. J Mass Dent Soc. 2006 Fall;55(3):40.
- Ogunlewe MO, Adeyemo WL, Ladeinde AL. Surgical management of a large complex odontoma of the mandibular angle-ramus region through intra-oral buccal approach–A case report. Niger Postgrad Med J. 2005 Dec;12(4):312-5.
- Chen Y, Li TJ, Gao Y. Ameloblastic fibroma and related lesions: a clinicopathologic study with reference to their nature and interrelationship. J Oral Pathol Med. 2005 Nov;34(10):588-95.
- Dhanuthai K, Kongin K. Ameloblastic fibro-odontoma: a case report. J Clin Pediatr Dent. 2004 Fall;29(1):75-7.
- Oghli AA, Scuto I, Ziegler C. A large ameloblastic fibro-odontoma of the right mandible. Med Oral Patol Oral Cir Bucal. 2007 Jan 1;12(1):E34-7.
- Gallana-Alvarez S, Mayorga-Jimenez F, Torres-Gomez FJ. Calcifying odontogenic cyst associated with complex odontoma: case report and review of the literature. Med Oral Patol Oral Cir Bucal. 2005 May-Jul;10(3):243-7.
- Praetorius F, Hjorting-Hansen E, Gorlin RJ, Vickers RA. Calcifying odontogenic cyst: range, variations and neoplastic potential. Acta Odonotol Scand 1981;39:227-240.
- Gorlin RJ, Pindborg JJ, Clausen FP, Vickers RA. The calcifying odontogenic cyst: a possible analogue of the cutaneous calcifying epithelioma of Malherbe. Oral Surg Oral Med Oral Pathol 1962;15:1235-1243.
- Hong SP, Ellis GL, Hartman KS. Calcifying odontogenic cyst: a review of ninety-nine cases with reevaluation of their nature as cysts or neoplasms, the nature of ghost cells, and subclassification. Oral Surg Oral Med Oral Pathol 1991;72:56-64.
- Batra P, Prasad S et al. Adenomatoid odontogenic tumour: review and case report. J Can Dent Assoc. 2005; 71:250-253.
- Philipsen HP, Birn H. The adenomatoid odontogenic tumor, ameloblastic adenomatoid tumor or adeno-ameloblastoma. Acta Pathol Microbiol Scand 1969; 75:375&ndash398.
- Philipsen HP, Reichart PA, Zhang KH, Nikai H, Yu QX. Adenomatoid odontogenic tumor: biologic profile based on 499 cases. J Oral Pathol Med 1991; 20:149–158.
- Sato D, Matsuzaka K et al. Adenomatoid odontogenic tumor arising from the mandibular molar region: a case report and review of the literature. Bull Tokyo Dent Coll. 2004; 45:223-227.
Sorry! you are incorrect
As mentioned previously, the clinical presentation including the age, location and the radiographic findings of multiple radiopaque masses simulating miniature teeth is almost pathognomonic for the clinical diagnosis of an odontoma. However, one should keep the differential diagnosis open and include other lesions such as benign neoplasms and cysts that can be associated with odontomas. For that reason, ameloblastic fibro-odontoma should be included on the differential diagnosis. The location of tooth #22 is highly unusual for ameloblastic fibro-odontoma. The histology is not supportive of this diagnosis either.
The ameloblastic fibroma is believed to have been described by Kruse in 1891. It is a relatively uncommon neoplasm. It is a benign, slow-growing, expansile, neoplasm or hamartoma of mixed epithelial and mesenchymal odontogenic origins. Some suggest that this lesion may represent an early stage of an odontoma. However, it behaves like a neoplasm in terms of growth and expansion of the jaw bones. It is known to inhibit tooth eruption and is therefore often associated with impacted teeth. It can also displace teeth. Therefore, these lesions can go undetected by parents unless a noticeable expansion occurs or because of failure of tooth eruption and displacement of teeth. It is rarely painful. It occurs most commonly in children in the first and second decade of life with an age range of infancy to 42 years of age. It has equal gender predilection and is more common in the posterior mandible than in the maxilla. It also occurs more often in the posterior jaws than in the anterior jaws. Radiographic findings include an impacted/unerupted tooth with a well-defined, usually unilocular radiolucency around the crown of a tooth, similar to a dentigerous cyst. It may also present as a radiolucency containing radiopaque material ranging from flecks to small tooth-like structures. Because of the continued slow growth, this lesion can reach very large sizes if left untreated. The histology of ameloblastic fibro-odontoma is made up of mixed epithelial and mesenchymal components. The epithelial component presents in the form of small islands, cords and rosettes of epithelial cells with columnar and palisaded peripheries and with centers that may or may not contain stellate or cuboidal epithelial cells. The mesenchymal component is made up of primitive connective tissue stroma with tooth-like hard material that has the features of a complex odontoma. They are benign and well-differentiated neoplasms; for that reason, transformation is rarely described. Conservative curettage and enucleaction is the treatment of choice, and there is a very low recurrence rate. The involved tooth is usually extracted. It has a good prognosis.
Sorry! you are incorrect
The patient is a little young for a calcifying odontogenic cyst, but the clinical and radiographic findings are consistent with it, especially with those associated with odontomas. For that reason, it should be considered on the differential diagnosis. The histology, however, is not supportive of this diagnosis.
Calcifying odontogenic cyst (COC) constitutes around 1% of all odontogenic cysts. Praetorius et al were the first to classify COC into two types: a simple cyst and a solid neoplastic spectrum. They classified the cystic type into subtypes A, B and C: A denoting a simple cyst, B an odontome-producing cyst, and C a cyst with ameloblastomatous proliferating. COC tends to occur around the third decade, with a patient age range of 7-82 years. It occurs equally in the maxilla and mandible, usually anterior to the first permanent molar, though it has a predilection for occurrence in the maxilla in the younger age range. It occurs equally in males and females. COC occurs more commonly in bone, but it can also occur in soft tissue (in the gingiva without a bony component, also known as peripheral COC). The peripheral counterpart of both lesions is less aggressive than the intra-osseous type. Histologically, COC can present in several ways: as a simple cyst with ghost cells and focal ameloblastoma-like epithelial changes, with more proliferative epithelium and ghost cells, with calcifications (both amorphous, tooth-like and calcified ghost cells), or as a true odontoma associated with such a cyst. Radiographically, COCs tend to be well-defined radiolucencies with occasional small radiopacities. They can be present at the apex, between teeth, or associated with impacted teeth. Clinically, COC can both expand the jaws and extend into the surrounding soft tissues and even the maxillary sinus. It can also resorb and displace teeth. The treatment of choice is thorough curettage.
Sorry! you are incorrect
The age of this patient, the location in the anterior mandible, and the association with impacted tooth #22 are all reasons to include adenomatoid odontogenic tumor (AOT) on the differential diagnosis. However, the presence of true, solid radiopaque masses simulating tooth-like structures (rather than simply flecks of calcified material) is highly unusual for AOT, rendering AOT a very unlikely diagnosis. The histology is not supportive of AOT.
Adenomatoid odontogenic tumor (AOT) is a rare neoplasm (hamartoma) accounting for fewer than 3% of all odontogenic tumors. It is benign and slow-growing and is believed to originate from the remnants of the dental lamina or enamel organ. It was first described by Dreibladt, in 1907, as a pseudoadenoameloblastoma. In 1969, Philipsen et al proposed the name adenomatoid odontogenic tumor, which was later adopted by the World Health Organization with the understanding that this lesion has a benign and non-aggressive behavior. It presents within bone (intra-osseous) in 97.2% of cases and on the gingiva (extra-osseous, also known as peripheral) in 2.8% of cases. The intra-osseous type is further divided into follicular and extra-follicular types. The follicular type accounts for 73% of all AOT cases and is associated with the crown of an unerupted/impacted tooth, sharing the same radiographic features as a dentigerous cyst. It is a unilocular, corticated radiolucency around the crown and at times goes beyond the crown to involve the root of the tooth. The extra-follicular type constitutes about 24% of cases, presenting between teeth, apically, or away from teeth. This type presents as a unilocular corticated radiolucency often mistaken for an odontogenic keratocyst, or lateral periodontal, residual or periapical cysts. This case would be classified as follicular in type. The peripheral variant presents on the gingiva, mimicking a reactive gingival swelling. Anterior maxilla and mandible are the most common locations for AOT; cases in the maxilla outnumber those in the mandible by a ratio of two to one, and the maxillary canines in particular account for 40% of cases. It has also been described in the posterior mandible and maxilla, but less commonly (9, 11). It is rarely described in deciduous teeth. It is more common in females (2:1 female-to-male ratio) between the ages of 10-19, with almost 70% of cases occurring in the second decade. Sizes are usually small, around 1-3 cm in diameter; occasionally, however, large lesions are described. Radiographically, it is usually unilocular and radiolucent with clearly defined to corticated margins. About 10% demonstrate some degree of calcification. AOT is usually an asymptomatic lesion with the exception of mild expansion. The extra-follicular type may cause mild displacement of teeth. Root resorption is rarely described. Histologically, it is made up of epithelial cells arranged in two patterns: some are spindle-shaped, arranged in whorls, nests and bundles, and others are cuboidal and arranged in duct-like structures. This lesion is supported a by thick fibrous connective tissue capsule. Sometimes globules of a homogenous material are described, which may represent amyloid. The treatment of choice is conservative removal through simple curettage or enucleation. The thick connective tissue capsule makes separation of the lesion from the tooth and surrounding connective tissue easy, allowing the clinician to save the tooth. Recurrence has been described but is exceedingly rare.