Large Exophytic Vascular Swelling, Area of Teeth #s 17 & 18
Can you make the correct diagnosis?
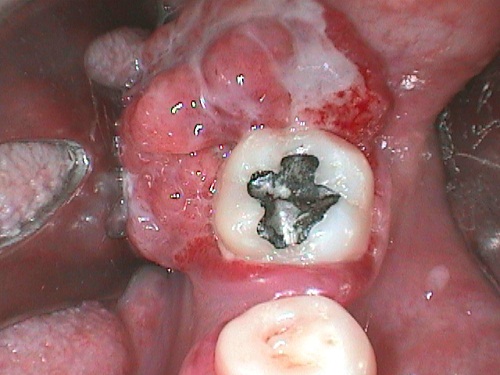
This is a 30-year-old Hispanic male who had had a fast-growing swelling over the six to eight weeks prior to his visit.
Congratulations! You are correct
The fast-growing, easily bleeding, exophytic gingival swelling is diagnostic of pyogenic granuloma and, for that reason, PG should be listed high on the differential diagnosis. The large size is unusual but is described. The histology is that of PG.
Pyogenic granuloma constitutes 85% of all reactive gingival swellings but can occur in areas other than the gingiva. It represents a profuse mass of vascular granulation tissue. It can be induced by trauma and local irritants such as excessive plaque, sharp fillings and dental calculus; it sometimes forms in an extraction socket in response to an irritant left in the socket. It can occur anywhere in the oral cavity and skin, especially the tongue, lips, fingers and nail beds. In the mouth, it occurs most commonly in the gingiva, especially the maxillary buccal and interproximal gingiva. Occasionally, it may surround the tooth. It is usually highly vascular, fast-growing, exophytic, lobular, sessile, and ulcerated or covered by pseudomembrane. The color changes from red to pink when it starts to heal. It occurs at any age and sex with a slight predilection for young females; it affects 1% of pregnant females. Pyogenic granuloma is usually painless except during eating, when bleeding and pain is described. Histologically, it presents as a mass of loose and vascular granulation tissue, usually with ulcerated or eroded surface epithelium and many inflammatory cells. A range of treatment modalities are available, including excision with removal of the local irritant, laser surgery, or intralesional injection with absolute alcohol, steroids or botulinum toxin. Scaling and polishing prior to surgical removal helps shrink the lesion. The prognosis is good, although recurrence is possible, especially during pregnancy.
References
- Fantasia JE, Damm DD. Red nodular lesion of tongue. Pyogenic granuloma. Gen Dent. 2003 Mar-Apr;51(2):190-194.
- Ichimiya M, Yoshikawa Y, Hamamoto Y, Muto M. Successful treatment of pyogenic granuloma with injection of absolute ethanol. J Dermatol. 2004 Apr;31(4):342-4.
- Pham J, Yin S, Morgan M, Stucker F, Nathan CA. Botulinum toxin: helpful adjunct to early resolution of laryngeal granulomas. J Laryngol Otol. 2004 Oct;118(10):781-5.
- Flaitz CM, Peripheral giant cell granuloma: a potentially aggressive lesion in children. Pediatr Dent. 2000 May-Jun;22(3):232-3.
- Chaparro-Avendano AV, Berini-Aytes L, Gay-Escoda C. Peripheral giant cell granuloma. A report of five cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2005 Jan-Feb;10(1):53-7; 48-52.
- Neville BW, Damm DD, Allen CM, Bouquot JE. Peripheral giant cell granuloma. In: Oral and Maxillofacial Pathology, 2nd edition. Philadelphia: W.B. Saunders, 2002. p. 449-451.
- Chigurupati R, Alfatooni A, Myall RW, Hawkins D, Oda D. Orofacial rhabdomyosarcoma in neonates and young children: a review of literature and management of four cases. Oral Oncol. 2002 Jul;38(5):508-15.
- Fatusi OA, Ajike SO, Olateju SO, Adebayo AT, Gbolahan OO, Ogunmuyiwa SA. Clinico-epidemiological analysis of orofacial rhabdomyosarcoma in a Nigerian population. Int J Oral Maxillofac Surg. 2009 Mar;38(3):256-60.
- McDonald MW, Esiashvili N, George BA, Katzenstein HM, Olson TA, Rapkin LB, Marcus RB Jr. Intensity-modulated radiotherapy with use of cone-down boost for pediatric head-and-neck rhabdomyosarcoma. Int J Radiat Oncol Biol Phys. 2008 Nov 1;72(3):884-91.
- Neville BW, Damm DD, Allen CM, Bouquot JE. Metastasis to the oral soft tissue. In: Oral and Maxillofacial Pathology, 3rd edition. Philadelphia: W.B. Saunders, 2007.
- Ogunyemi O, Rojas A, Hematpour K, Rogers D, Head C, Bennett C. Metastasis of genitourinary tumors to the head and neck region. Eur Arch Otorhinolaryngol. 2009.
Sorry! you are incorrect
The third most common gingival swelling is peripheral giant cell granuloma (PGCG). The color, the fast growth, the location and the age of the patient are all potentially indicative of a diagnosis of PGCG. The histology, however, is not supportive of a diagnosis of PGCG.
Peripheral giant cell granuloma constitutes fewer than 5% of all reactive gingival swellings. It consists of a hyperplastic mass of vascular granulation tissue with many osteoclast-like multinucleated giant cells. It presents as a lobular, purplish-blue exophytic nodule exclusively on the gingiva, both edentulous and dentate, and usually anterior to the molars. It originates from either the periodontal ligament or the periosteum. It occurs across a wide age range, especially in children, young adults, and females (2:1 female-to-male ratio). It presents as either sessile or pedunculated and smooth-surfaced or lobular. Though usually painless, it can occasionally be ulcerated, painful and accompanied by bleeding. Like pyogenic granuloma, it is usually present either on the buccal or lingual gingiva or between teeth, but it can occasionally surround the teeth and act aggressively by displacing teeth much like a sarcoma. It can also resorb the underlying bone in a smooth and concave “saucer-like” manner. Complete excision including curettage of underlying bone is the preferred treatment. It has a good prognosis with a recurrence rate of approximately 10%.
Sorry! you are incorrect
The fast-growing nature of this specimen combined with the gender should make one think of conditions beyond the obvious reactive gingival swellings. Rare conditions such as sarcomas are potential lesions to be considered on the differential diagnosis. The fast growth and fleshy, bulbous clinical presentation is consistent with the behavior of a sarcoma, especially rhabdomyosarcoma. The age of the patient, however, is unusual except in the case of pleomorphic rhabdomyosarcoma. The histology is not supportive of any sarcoma.
Rhabdomyosarcomas are malignant neoplasms of skeletal muscle origin constituting 4–8% of all malignancies in children under the age of 15. They most commonly occur in the head and neck (35%), followed by the genitourinary tract (23%) and the extremities (17%). In the head and neck area, the orbit is the most common location, followed by the nasal cavity, oropharynx and the oral cavity. Occurrences in the mouth account for 10–12% of all head and neck rhabdomyosarcomas. The tongue, palate and cheek are the most common sites of occurrence in the oral cavity. Clinical presentations of rhabdomyosarcomas vary, ranging from small and exophytic to ulcerated, fungating and fast-growing lesions. Rhabdomyosarcomas can occasionally be associated with pain, trismus, paresthesia, facial palsy, and/or aural or nasal discharge. The variations in the clinical presentation can lead to delayed diagnosis. Three histologic types are described: embryonal, alveolar and pleomorphic. Embryonal and alveolar rhabdomyosarcoma are most common in children while pleomorphic rhabdomyosarcoma is most common in adults, though it is rare after the age of 45. They can also occur at birth; these cases, known as congenital rhabdomyosarcomas, are exceedingly rare. They are treated with multi-drug intensified chemotherapy combined with radiotherapy and surgery. This treatment modality has improved the overall 5-year survival rate for the pediatric group from 25% in 1970 to 74% currently. Rhabdomyosarcomas can metastasize, usually to the lungs, bone, and brain.
Sorry! you are incorrect
Cancer metastasis to the mouth is exceedingly rare and the most common location for metastatic disease is the jaw, specifically the posterior mandible, followed by the gingiva. Given that this patient has no history of primary cancer, it would be highly unlikely that this lesion represents a metastatic disease. The histology is not supportive of a metastatic malignancy.
Cancer metastasis to the oral cavity is neither specific nor common. Although it constitutes fewer than 1% of all oral malignant neoplasms, it may have a devastating result to the patient mainly because metastasis to other sites has already developed or is inevitable. Theoretically, any malignant neoplasm can metastasize to the oral cavity, but in actuality few do and out of the ones that do, the majority are carcinomas rather than sarcomas. The most common malignant neoplasms that metastasize to the mouth are from the breast, lung, kidney and prostate. Malignant neoplasms from the thyroid, pancreas, colon, and liver have also been described. Breast cancer is the most common neoplasm to metastasize to the oral cavity regardless of gender. However, lung and prostate cancers are the most common neoplasms to metastasize to the oral cavity in men. In the most cases, the oral presentation is a secondary diagnosis when the primary diagnosis of the distant organ has been already made and the patient has had or is undergoing treatment for it. Although rare, it is occasionally the case that the oral lesion is the first manifestation of the disease. By far the most common location is the posterior mandible, where 80% of cases occur, followed by the gingiva. It is typically described in adults over the age of 30 and rarely in children. Pain and swelling are the most common clinical symptoms. It may also present as asymptomatic, simulating a periapical lesion, or it can cause anesthesia and parasthesia, especially when it involves the inferior alveolar canal. The latter results in so-called “numb-chin syndrome.” Tooth loosening, displacement and sharp resorption have also been described. Gingival swelling, like a pyogenic granuloma, has also been described. The radiographic appearance of irregular bony destruction is also common for metastatic tumors. The majority of neoplasms cause bony destruction with ill-defined borders, the moth-eaten appearance of some bony destruction indicating aggressive behavior. It is also important to mention that at times, well-demarcated lesions with a benign morphology, as well as cystic radiographic morphology, have also been described. Metastatic neoplasms from the prostate may also be bone-forming, resulting in either radiopaque or mixed radiopaque and radiolucent lesions misdiagnosed as a benign fibro-osseous lesion. The diagnosis of tumor metastasis to the oral cavity carries a poor prognosis because the oral cavity is usually not an isolated site and tends to project more disseminated clinical behavior. Patients are typically treated with chemotherapy and the five-year survival rate is very low.