Mandibular Cyst
Can you make the correct diagnosis?
This is a 12-year-old healthy Caucasian male who presented at his General Dentist office for a routine dental examination, radiographs and dental prophylaxis.
Congratulations! You are correct
While the main cause of a dental abscess in a child is a periapical lesion due to a badly carious or fractured and non-vital tooth, abscesses can occasionally be attributed to reasons other than these. Such is the case with a mandibular buccal infected cyst, also known as paradental cyst, and buccal bifurcation cyst. Mandibular buccal infected cyst is an inflammatory lesion involving the buccal and distalobuccal aspects of the mandibular permanent molars, and is usually attached to the cervical margins extending down to the root bifurcation (1). It rarely affects other teeth; it has been shown to involve the permanent premolar teeth (2). Although infected, often with suppuration, the associated teeth are vital. Some investigators believe that the paradental cyst is the same entity as buccal infected cyst that mainly affects a partially erupted mandibular third molar tooth. Several factors have been implicated in the origin of this cyst, including its origin from the epithelial rests of Malassez, the dental follicle around the erupting tooth, the crevicular epithelium, and the reduced enamel epithelium. Occasionally the involved tooth has a small enamel spur of pearl in the furcation area that may cause the inflammatory process (1-3). These cysts are frequently misdiagnosed as inflammatory dentigerous cysts, lateral radicular or lateral periodontal cysts (2-4). They affect children around 8-13 years of age, and are more common in males (1-4). Paradental variant tends to occur in older patients around 24 years of age. Patients usually present with buccal gingival swelling, pain, and at times a sinus tract releasing pus. These cysts are often bilateral, which was the case in this patient. Clinically the patient had the defect involving teeth #s 18 and 31. Radiographically, however, only tooth #31 showed the typical features.
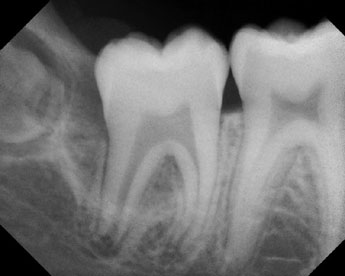
Radiographically, these cysts are readily diagnostic with specific features, including the presence of a periodontal defect buccal and distal to the involved tooth, buccal expansion of the buccal cortical bone. Teeth are displaced lingually and usually the adjacent non-erupted tooth shows no evidence of an increased follicular space. However, on occasions radiographic changes are not as readily detectable as is the case with tooth #18 in this case (Fig 3) where clinically the tooth had a defect probing 5-6 mm while radiographically no changes were detected. The histology is non-specific. It may be very similar to a radicular cyst, periodontitis or an inflamed dentigerous cyst. There is usually loose and vascular granulation tissue wall, lined by stratified squamous epithelium with intense inflammatory cells, and often with abscess formation. All of these features were present in the histologic specimen from our case. The treatment of choice is enucleation and preserving the involved tooth (1-4). The teeth usually grow normally. Recurrence is rare and may be attributed to incomplete removal of the lesion.
Treatment
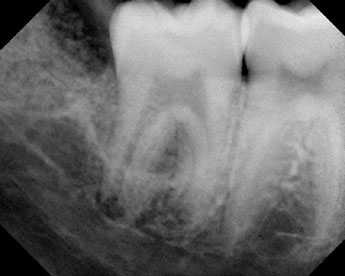
Flap surgery on tooth # 31 with curettage biopsy and the surgical extraction of tooth # 32 was performed on 05/28/2004. Following the extraction of tooth # 32 and curettage of the soft tissue (Fig 3), the osseous crater defect extending from the distal root surface of tooth # 31 and incorporating the third molar crown site was substantial. A mixture of mineralized freeze-dried bone allograft with tetracycline powder was placed to fill the space, providing a clotting medium and supporting the flaps by creating a full closure over the surgical site. A primary closure was achieved with the placement of four interrupted loop sutures. The tissue samples were submitted to the Oral Pathology Biopsy Service for a microscopic evaluation and a definitive diagnosis. The healing response was evaluated at one, two (sutures removed), four, eight and sixteen weeks. The early healing progressed without suppuration and new bone has progressively regenerated the base of the pocket. A Monoject 412 syringe has been used to irrigate the decreasing pocket and for debridement of trapped particles.
Figure 3. Area of tooth # 31 after treatment (view w/ graft).
References
- Graig, G. The paradental cyst: a specific inflammatory odontogenic cyst. Br Dent J. 1976; 141:9–14.
- Morimoto Y, Tanaka, T et al. Inflammatory paradental cyst (IPC) in the mandibular premolar region in children. Oral Surg Oral Path Oral Med. 2004; 97: 286-293.
- Thompson, IO, de Waal, J et al. Mandibular infected buccal cyst and paradental cyst: the same or separate entities? J Dent Assoc S Afr. 1997; 52: 503–506.
- Lim AA, Peck, RG. Bilateral mandibular cyst: lateral radicular cyst, paradental cyst, or mandibular infected buccal cyst? Report of a case. J Oral Maxillofac Surg. 2002; 60:825-827.
- Shaw, W, Smith, M et al. Inflammatory follicular cysts. ASDC J Dent Child. 1980, 47; 97–101.
- Shibata, Y, Asaumi, J et al. Radiographic examination of dentigerous cysts in the transitional dentition. Dentomaxillofac Radiol. 2004; 33:17-20.
- Hyomoto, M, Kawakami, M et al. Clinical conditions for eruption of maxillary canines and mandibular premolars associated with dentigerous cysts. Am J Orthod Dentofacial Orthop. 2003; 124:515-520.
- Jiunta JL. Gingival cysts in the adult. J Periodontol. 2002; 73:827-831.
Sorry! you are incorrect
Dentigerous cyst is the most common developmental cyst in the oral cavity accounting for 20% of cysts of the jaw, and is almost always associated with the crown of a tooth attached to the cemento-enamel junction. It is believed to originate from the accumulation of fluid between the reduced enamel epithelium and the tooth crown. Inflammatory dentigerous cyst (IDC) was first described by Shaw et al in 1980 to occur in mixed dentitions. He described the development of an enlarging follicular space around an unerupted permanent tooth with an overlying non-vital deciduous tooth. Shaw et al interpret the cyst to be the result of spread of periapical inflammation from the overlying non-vital primary tooth into the dental follicle of the permanent tooth below, leading to an inflammatory process and to the formation of a developmental cyst. The inflammatory dentigerous cysts most frequently occur in the mandibular premolar area. The clinical presentation of buccal infected cyst differs from that of an inflammatory dentigerous cyst. The buccal infected cyst presents with a periodontal defect buccal and distal to the involved tooth not seen in IDC. It is usually associated with an erupting tooth. The follicular space between the crown of the tooth and the dental follicle is expanded in a dentigerous cyst but not in the buccal infected cyst. Radiographically, IDCs can be similar to buccal infected cysts. However, they usually present as unilocular corticated (unless inflamed) radiolucency around the crown or can be lateral to a crown, but with a well-defined radiolucency. The histology, however, may be non-specific and similar to that of a buccal infected cyst, especially if the dentigerous cyst is infected. Treatment is simple curettage with good prognosis (4-7). Neither the clinical or radiographic findings are consistent with an inflammatory dentigerous cyst.
Sorry! you are incorrect
Lateral periodontal cyst (LPC) is an uncommon Odontogenic cyst, accounting for 2% of all jaw cysts. It occurs more commonly in the mandibular cuspid and bicuspid teeth area. It usually occurs in adult males older than 30 years of age. Because it is usually asymptomatic, LPC is often discovered during routine dental examinations. The involved teeth are vital. LPC presents as a small, well circumscribed, unilocular radiolucency located between the involved teeth. Histologically, a LPC has a distinct histology that can be diagnosed in the absence of any clinical or radiographic findings. It therefore cannot be mistaken for a buccal infected cyst (4, 8). Given the clinical, radiographic and histologic features, this cyst is not consistent with a LPC.
Sorry! you are incorrect
Lateral radicular cyst (LRC) is a variant of a periapical (radicular) cyst associated with a non-vital tooth. Varying in its location, LRC is located to one side (lateral) of a tooth rather than apical. Radiographically, the features are similar to a periapical cyst. They are usually less than 1 cm in size and can be corticated depending on the degree of inflammation (4). Histologically, LRC is non-specific inflamed fibrous or connective tissue with or without lining epithelium. The fact that the associated tooth was vital excludes the diagnosis of a lateral radicular cyst.